Advances in cancer care have improved cancer patients’ chance of survival. But some cancer treatments, while successful at treating cancer, may impact patients’ heart health.
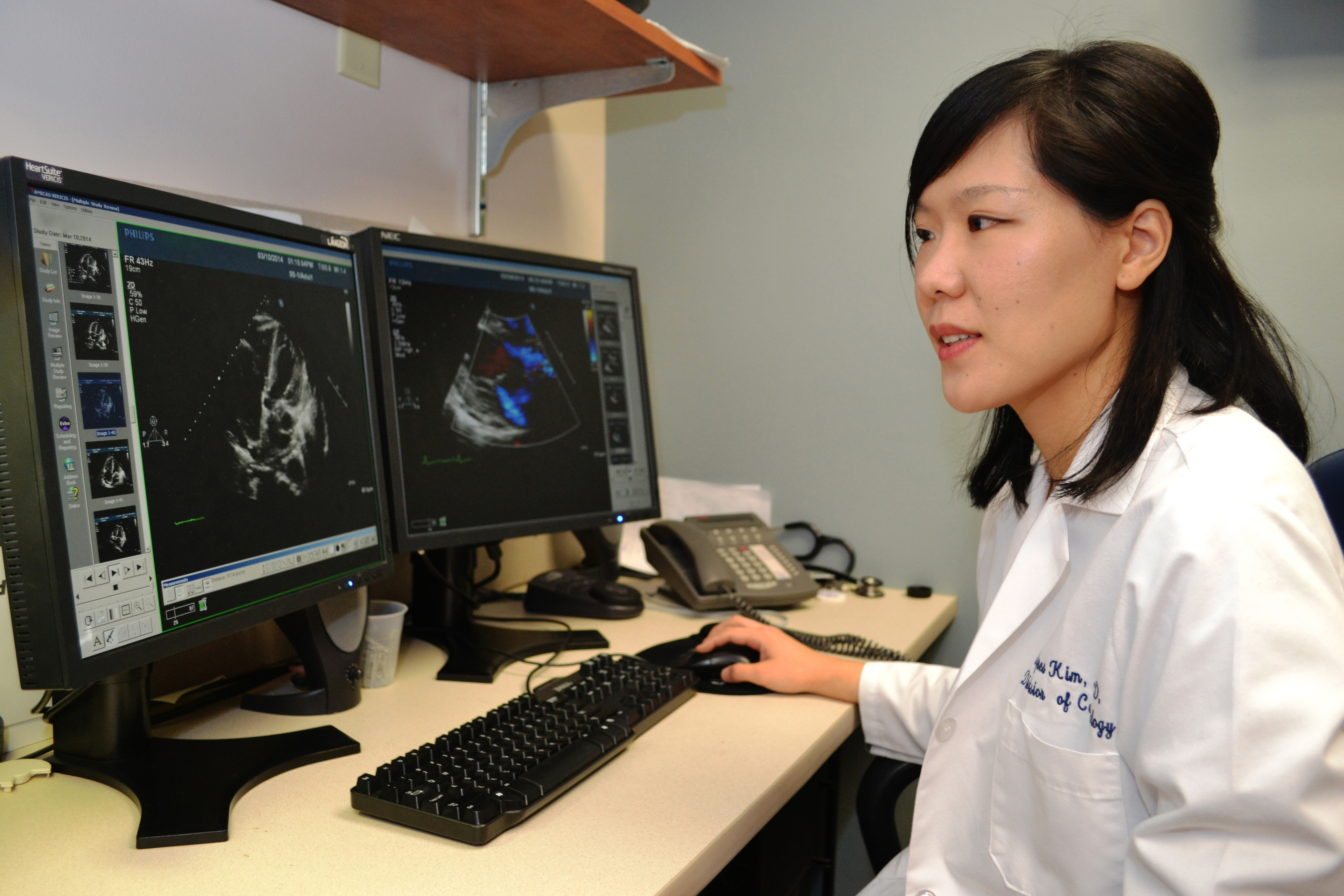
This Heart Month, Dr. Agnes Kim, director of the Cardio-Oncology Program at UConn Health, discusses what you need to know about protecting your heart during cancer care.
How might cancer treatment affect your heart?
Chemotherapy or radiation treatments are often used to treat and cure cancer, but also may cause damage to your heart or blood vessels. These potential side effects are known as cardiotoxicity. Cardiotoxicity can develop during cancer treatment, occur within days or months, or may even manifest years after successful cancer treatment, potentially impacting quality of life and life expectancy.
What is cardio-oncology?
As cancer survival rates continue to increase, knowledge about cardiotoxicity related to cancer treatment has been growing. The goal of the Cardio-Oncology Program at UConn Health is to detect, prevent, and manage cardiotoxicity so that patients can successfully complete their cancer treatment without untoward damage to their heart. Also, researchers are working to learn more about what causes cardiotoxicity from cancer care and how it can be better detected, treated, and prevented.
The Cardio-Oncology Program includes multidisciplinary specialists from the Pat and Jim Calhoun Cardiology Center and the Carole and Ray Neag Comprehensive Cancer Center to prevent or minimize a patient’s risk of heart damage during and after treatment. The program also evaluates and manages patients who have had cancer treatment in the past and develop new cardiac symptoms or problems.
How might chemotherapy affect the heart?
Certain chemotherapy drugs can damage the heart muscle, causing it to pump less effectively, and potentially leading to heart failure. Other cardiotoxic effects related to cancer chemotherapy are myocarditis/pericarditis (inflammation of the heart muscle and the sac surrounding the heart), reduced blood flow to the heart (myocardial ischemia), low blood pressure (hypotension), high blood pressure (hypertension), abnormal heart rhythm (arrhythmia), and increased risk for blood clots (thrombosis).
How does radiation therapy affect the heart?
Radiation therapy to the chest, which is often part of the treatment for Hodgkin’s lymphoma and cancers of the lung, esophagus, or breast, can affect many aspects of the heart. Radiation can injure the pericardium (the tissue covering the heart), heart valves, the heart muscle itself, coronary arteries, and the heart’s electrical system. The risk of cardiotoxicity from radiation therapy increases with higher doses, and usually manifests many years to decades after exposure.
Who is most at risk for chemotherapy or radiation damage to the heart?
Those cancer patients at highest risk for cardiotoxicity include:
- Patients with existing heart disease even before they start cancer treatment.
- Patients who receive a combination of chemotherapy and radiation therapy to the chest.
- Patients who are being treated with high-risk drugs (i.e. a class of medications called anthracyclines, or trastuzumab).
- Patients with cardiac risk factors such as hypertension, diabetes, high cholesterol, obesity, who are smokers, or have a strong family history of cardiac disease.
What steps do you advise that cancer patients take to protect their heart?
Ask your doctor if your cancer treatment plan includes any cancer drugs or radiation therapy that can pose a risk to your heart and blood vessels.
If the answer is yes, talk to your doctor about having a thorough cardiac evaluation before, during, and after cancer treatment.
Also, keep notes of the types and doses of drugs and radiation therapy that you will receive. Eat healthy, quit smoking, and take exercise. Importantly, tell your doctor about any shortness of breath, swelling of legs, chest pain, or heart palpitations, which could be warning signs of a heart issue developing.