As the days lengthen and you spend more time in the sun, spare some thought for your skin. Melanoma is one of the deadliest types of skin cancer and it’s becoming more common, especially in young adults. But doctors can’t always tell from a biopsy which melanomas are the most dangerous. Now UConn Health researchers have found a molecular signal that could distinguish which skin cancers need more aggressive treatment. Their findings, reported in the February issue of Laboratory Investigation, may also explain the real reason why exposure to ultraviolet light increases the odds of skin cancer.
The big question in skin cancer is why some melanomas spread aggressively, and others don’t. — Sam Dadras
Melanomas usually manifest as dark, unevenly colored moles on the skin (see sidebar). Dermatologists judge how dangerous the cancer is by how thick it is and how deeply it has penetrated. But that’s only a rough estimate. Some thick melanomas haven’t spread and are easy to remove, while some smaller cancers have already seeded themselves throughout the body. The big question in skin cancer is why some melanomas spread aggressively, and others don’t.
Two patients with melanomas of the same depth can have very different outcomes, according to UConn Health dermapathologist Sam Dadras. “Depth is not necessarily reliable; a molecular approach might be a better approach,” for judging how to treat a skin cancer, he says.
Dadras and his colleagues wondered if there was a molecular signature of aggressive cancer. Did the most dangerous cancers produce different molecules than less dangerous ones? They began measuring micro-ribonucleic acid (micro-RNA) levels in melanomas. RNA acts as a messenger that translates the instructions in a cell’s DNA into actual proteins. Micro-RNAs are like little caps that seek out and cover up other RNAs, preventing them from making proteins. The type of micro-RNAs can significantly change the kinds of proteins available to a cell – and that can change a cell’s behavior. For example, a cell might have genes that prevent it from turning cancerous. But if micro-RNAs suppress the anti-cancer proteins those genes make, the cell can go rogue anyway.
The researchers began sampling the micro-RNAs in melanomas and then comparing them to the micro-RNAs found in non-cancerous moles in the same person. They found about 40 micro-RNAs were significantly different between melanomas and normal moles. Then they took 167 different melanoma samples and analyzed those top 40 micro-RNAs. And they found a striking signature: aggressively invasive melanomas had higher levels of micro-RNA21 and lower levels of micro-RNA let7b than less advanced melanomas. It made sense, as micro-RNA21’s target is a gene known to suppress melanoma tumor growth. As micro-RNA21 levels increase, that gene is suppressed even more and the tumor can grow faster.
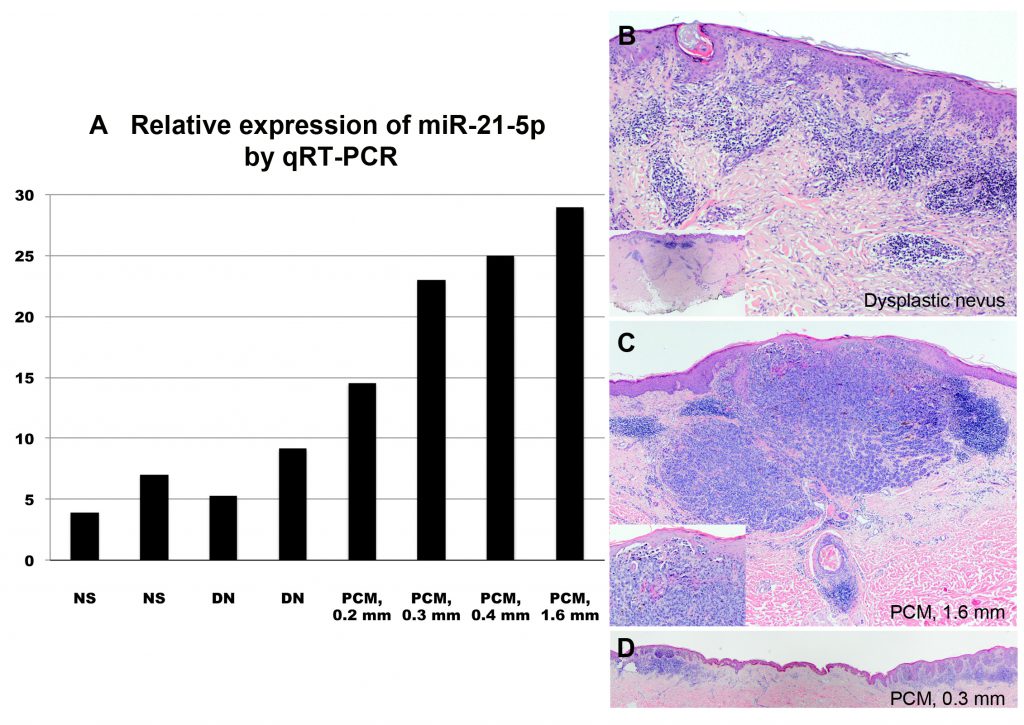
So this molecular signature exists, and could potentially help doctors identify which patients should opt for more aggressive cancer treatments. But Dadras and his colleagues also wondered how the micro-RNA differences originally came about.
“There’s no studies linking DNA damage from UV to melanoma,” Dadras says. It’s well-established that sun and ultraviolet light exposure is a risk factor for skin cancer, but not because exposure directly damages DNA. Or RNA, for that matter.
How does sunlight change the micro-RNA in a cell? The evidence suggests that ultraviolet light from the sun and from tanning beds changes the micro-RNA expression in keratinocytes, the cells that make pigment in our skin. It doesn’t directly damage the DNA, but rather changes which genes – and so which micro-RNAs – are expressed. So the researchers propose that the keratinocytes exposed to ultraviolet light start making more micro-RNA21, which inactivates the tumor suppresser gene, which leads to tumor growth.
So next time you’re outside enjoying the sun, appreciate all the complex things happening in your skin. And don’t forget to wear sunscreen.