Lab tests for COVID-19 require pricey equipment, and field tests aren’t globally available nor work in real-time, making it hard for health care workers in remote areas of the globe to diagnose the disease. To help, UConn researchers have invented a portable, inexpensive device that has the potential to diagnose COVID anywhere.
Getting tested for COVID-19 is easy in Connecticut, where clinics, hospitals, and pharmacies have free testing stations, and even at the height of the pandemic most people could get tested fairly quickly. But in many other parts of the world, it’s not so easy. There aren’t always labs with the right equipment nearby, and field portable tests’ results aren’t available immediately.
UConn engineering professor Bahram Javidi and biomedical engineering graduate student Timothy O’Connor had an idea for a better, easier way to test for COVID. They knew red blood cells are affected during a bout of COVID-19. Red blood cells carry oxygen from your lungs through your bloodstream to all parts of your body, and many of the symptoms of COVID-19, including low oxygen levels and blood clots, involve red blood cells.
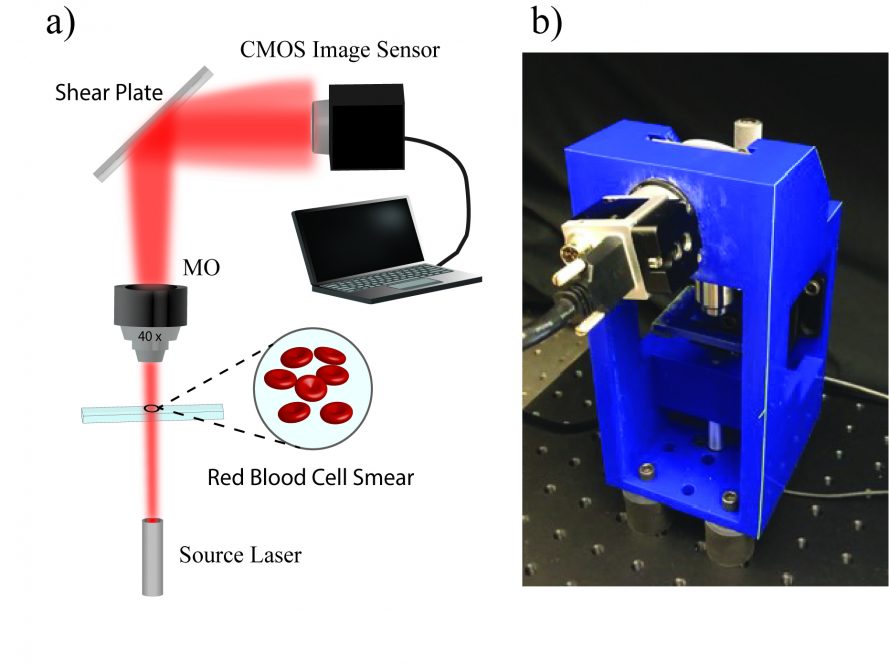
They suspected they might be able to diagnose COVID by shining laser light on a sample of red blood cells and seeing how the light changed as it propagated through them: red blood cells with COVID might leave a measurable signature in the light. Laser light had been used to diagnose other diseases involving red blood cells before.
To understand why this would work, remember that lasers are a special form of light. Unlike the sun’s light, which shines in all colors, a laser shines in a single, very specific color. And all the light from a laser can be made to travel in the same direction and at the same speed. But when this uniform beam of laser light has to pass through something such as a red blood cell, it changes. The light scatters in different directions, changes speed, or bends a little, producing small changes in the affected light waves. And a sick red blood cell that’s a little changed biochemically, or misshapen, could change the light beam’s characteristics in a different way than a healthy blood cell would.
Such changes can be subtle and hard to detect with the naked eye. So Javidi and O’Connor used a machine learning technique to have a computer detect how the variations in the laser light differed between healthy and COVID-positive red blood cells. UConn Health School of Medicine Dean Bruce Liang and physiologist Jian-Bing Shen collaborated by supplying red blood cells donated by UConn Health COVID patients, and helped with the completion of the project.
The machine learning process worked, and Javidi and O’Connor were able to reliably train a computer to distinguish between healthy and diseased cells. They describe their work in the 5 May issue of Optics Letters.
Armed with that that information, they could hook up an inexpensive laser and a portable 3D holographic microscope to a laptop to create their COVID diagnostic device. The device can actually be constructed with a 3D printer. And anyone who can take a finger prick’s worth of blood and smear it on a glass microscope slide can be trained to use the device to diagnose COVID-19.
The team admits there is one weakness in their testing: so far, all the red blood cell samples they’ve used were from COVID-19 patients sick enough to be hospitalized. They would like to test the device on red blood cells from people who have mild or asymptomatic cases, and are looking for health care providers and researchers in Connecticut, Massachusetts, elsewhere in the country, and around the world to work with them.
This research was funded by the UConn Office of the Vice President of Research.