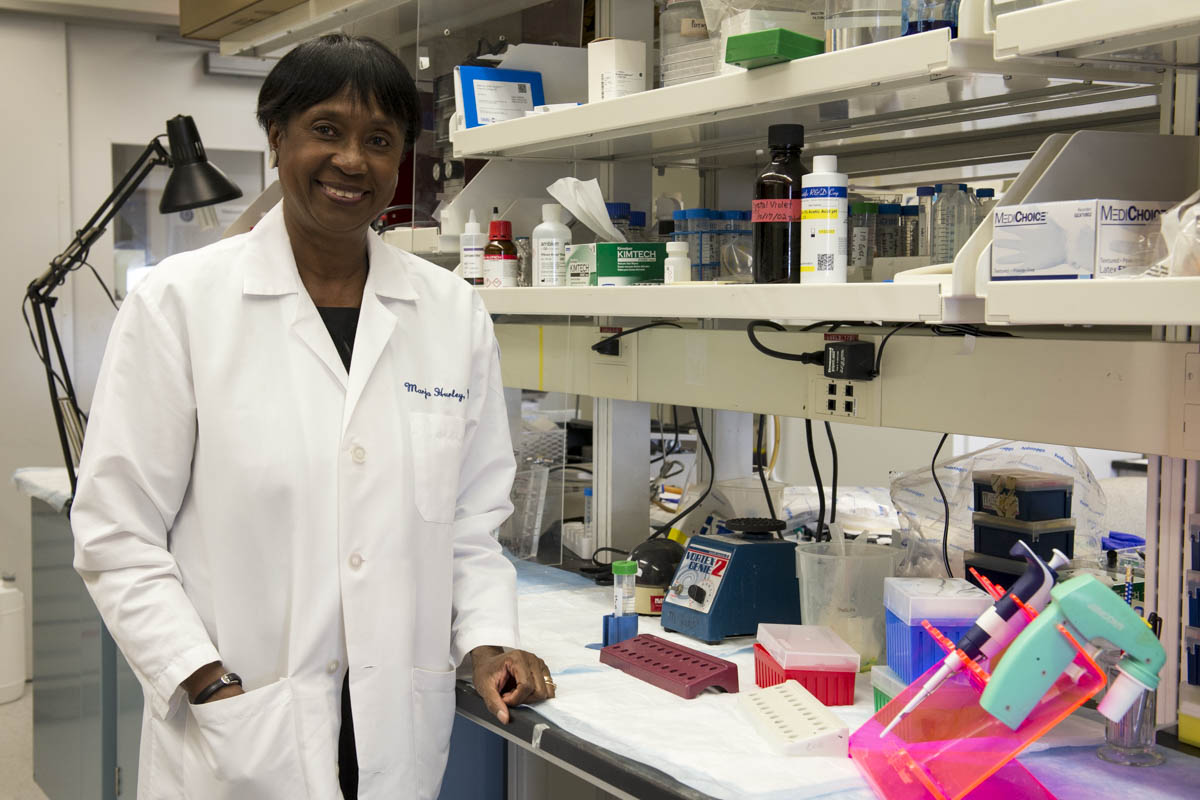
In honor of World Sickle Cell Day, marked each June 19, we share that UConn Health’s Dr. Marja Hurley has recently received nearly $3 million in research funding from the NIH and a pharmaceutical company to advance scientific knowledge about sickle cell disease and its related bone loss.
Hurley, a pioneering physician-scientist, is renowned for her three decades of NIH-funded bone research. She is a UConn Board of Trustees Distinguished Professor of Medicine and Orthopedic Surgery at UConn Health.
Sickle cell disease is a painful inherited red blood cell condition impacting the blood’s circulation due to abnormally hook-shaped red blood cells. Individuals born with the disease have severe pain episodes due to blockages that can form inside their smaller blood vessels, capillaries, and even bone marrow, when their abnormally shaped cells cannot pass through smoothly. The dangerous blockages can reduce blood flow, may cause deadly blood infections, or profound anemia, an unhealthy level of oxygen-rich red blood cells.
While the sickling of red blood cells inside bone marrow causes severe bone pain episodes it also can cause bone infarctions or damaged areas. However, little is known why a high prevalence of sickle cell patients also experience musculoskeletal frailty and brittle and broken bone complications such as osteoporosis.
To study this phenomena The National Institute of Diabetes and Digestive and Kidney Diseases has awarded a 4-year $2,211,239 grant to Hurley as principal investigator with co-investigators Dr. Liping Xiao, assistant professor of medicine and psychiatry, and Siu-Pok Yee, Ph.D, associate professor of cell biology at UConn School of Medicine.
Together the research team will study how sickle cell disease contributes to impaired bone mineralization. Specifically, the researchers will research in mouse models the molecular mechanism impacting the phosphate regulating hormone Fibroblast Growth Factor 23 (FGF23). These studies will aim to identify whether FGF23 is a novel contributor to the pathogenesis of sickle cell disease-related bone loss and anemia and if it can be prevented in the laboratory with the findings translated someday to patient care.
“Our hope is that we can develop a useful therapy to prevent bone loss in sickle cell disease patients in the very near future,” stresses Hurley. “There is much needed intervention to further fuel scientific discoveries to not only curb the pain suffered by sickle cell patients but further enhance their overall musculoskeletal health and well-being.”
In addition, the pharmaceutical company, Global Blood Therapeutics (GBT), has provided Hurley with a 3-year $535,000 grant to study bone and muscle function in sickle cell disease mouse models.
The drug Voxelotor is a currently FDA-approved drug for treatment for the anemia caused by sickle cell disease. However, little has been determined about the efficacy of the drug to also increase muscle strength and bone mineral density in sickle cell disease patients or mouse models. Hurley’s research will be investigating this drug’s promise further.
More than 3.5 million are affected worldwide by sickle cell disease, including approximately 100,000 Americans, and in Connecticut, at least 1,000 adults and 600 children. African-Americans and Latinos are predominantly affected in the U.S., with life expectancy for the majority of people with sickle cell disease is now age 40 or greater thanks to advanced health management.