Researchers in the Department of Biomedical Engineering —a shared department between the UConn Schools of Dental Medicine, Medicine, and Engineering—unlocked a new strategy using sugar molecules to thermally stabilize their existing microneedle vaccine technology, eliminating the need for cold-chain storage.
Associate Professor Thanh Duc Nguyen from the Departments of Mechanical Engineering and Biomedical Engineering in the School of Engineering, reported this new development in a recent issue of Advanced Materials Technology. The work was led by Dr. Khanh Tran, Nguyen’s former UConn Ph.D. student currently at the Massachusetts Institute of Technology, and Dr. Tyler Gavitt, former UConn Ph.D. student currently at Duke University. Gavitt was a student of Associate Professor Steven Szczepanek in the Department of Pathobiology and Veterinary Science in the College of Agriculture, Health and Natural Resources at UConn.
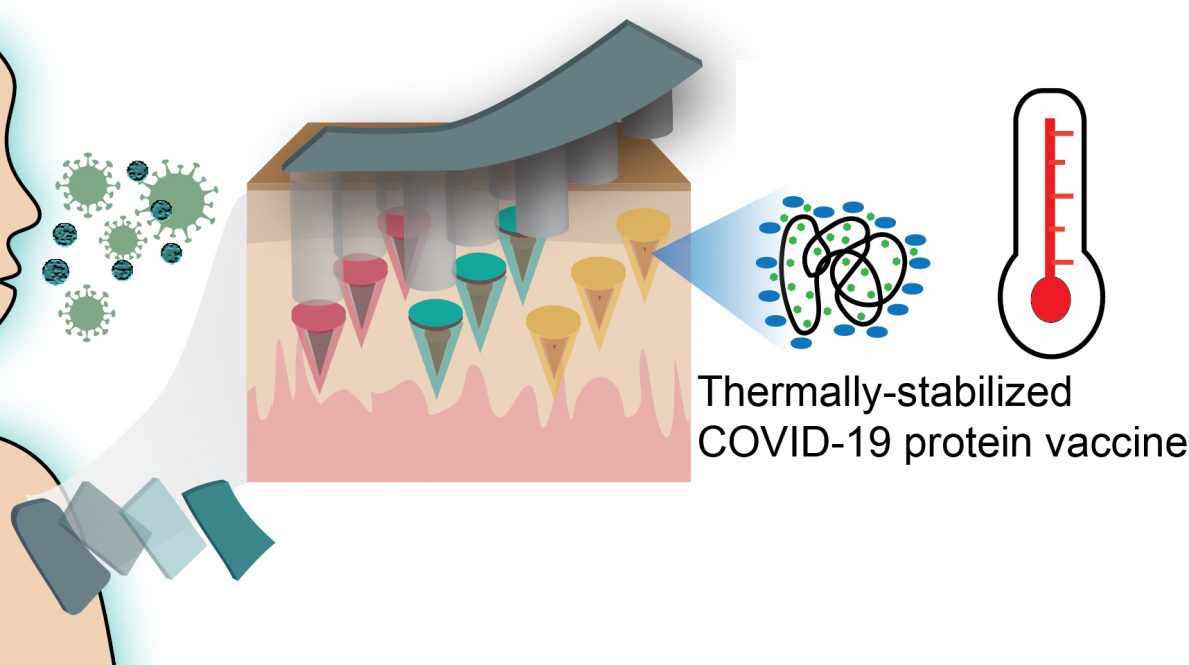
Typically, vaccinations against infectious diseases like COVID-19 require multiple painful, expensive and inconvenient injections, including a prime and several booster shots. The UConn researcher’s technology creates a self-administered microneedle patch which could be self-administered and only requires a single-time administration into skin—similar to a nicotine patch—to perform a release profile of vaccines, simulating the effect of multiple injections.
The necessity for cold-chain storage, however, is an added logistical hurdle for vaccine distribution.
“While mRNA vaccines can be quickly designed and manufactured to tackle the pandemic viruses like the COVID-19, the global vaccination campaigns need a more traditional protein-based vaccine so that it can be manufactured at a larger scale with already-built vaccine-manufacturing facilities around the world for a global distribution,” says Nguyen. “Unfortunately, these protein-based vaccines, similar to mRNA, are very unstable under heat and need to be stored at cold temperatures below – 80oC in expensive freezers. This becomes a significant logistic burden for vaccines transportation and distribution as many developing countries and rural/remote areas around the world cannot afford such cold-chain storage conditions.”
The researchers identified the sugar molecules trehalose and sucrose as two key ingredients to help stabilize the recombinant SARS-CoV-2 S1-RBD protein antigen—the protein projected from the shell of COVID-19 virus. In water-based environments, a protein’s 3D structure can misfold at high temperatures—similar to how an egg white hardens as you poach it. This would ruin a vaccine antigen protein. Proteins in a dried form will be more stable, but removing water carelessly can also destroy the protein’s structure. The researchers selected trehalose and sucrose because of their ability to serve as water substitutes and form hydrogen bonds with the proteins to prevent the protein mis-folding. The highly viscous sugar environment can also help to minimize protein mobility and exposure to the environment, protecting from further destabilization.
In the study, the researchers mixed the trehalose-sucrose solution at several different ratios with the recombinant SARS-CoV-2 S1-RBD protein and vacuum-dried the mixture overnight. The samples were exposed to heat for one-hour short-term stability screenings, and then body temperature for long-term stability for 2, 4, 8, 12, and 16 weeks. The researchers were able to confirm that with this formulation that their vaccine technology can be stored at extreme temperatures for at least one hour, and body temperatures for at least four months. This is the first reported effort to stabilize the specific recombinant SARS-CoV-2 S1-RBD protein with trehalose and sucrose formulations.
“Loading of the microneedles patches with stabilized recombinant SARS-CoV-2 S1-RBD protein induced both binding and functional neutralizing antibody responses in rats against different strains of SARS-CoV-2 virus, thus demonstrating the potential of this technology to being a viable needle-free alternative to the traditional vaccination paradigms. This could revolutionize the vaccination process worldwide by avoiding repeated injections, trained medical personnel, and cold-chain facilities for vaccine storage” Tran says.
The researchers initially received a $432,990 contract from the U.S. Department of Health and Human Services (HHS) BARDA to develop the microneedle vaccine technology. In addition to the funding from BARDA, the researchers received $160,000 from the University of Connecticut to share the cost of the project. Nguyen also co-founded a spin-off company, SingleTimeMicroneedles Inc., to commercialize this microneedle platform with the assistance of UConn’s Technology Commercialization services.