Anyone who has had to move knows what a pain it is. But imagine not just moving geographically, but switching between completely different biological environments with different nutrients available and immune systems working against you – well that’s the life cycle of Borrelia burgdorferi the bacteria that causes Lyme disease.
The most prevalent arthropod-borne infection in the United States, the Center for Disease Control reports there are 300,000 cases of Lyme disease annually.
First discovered in Lyme, Connecticut, this disease is particularly prevalent in the northeast.
“Humans get infected when they go into a place where the cycle is going on. It doesn’t have to be deep in the woods, it can be in your backyard,” says Justin Radolf, a UConn Health professor of medicine.
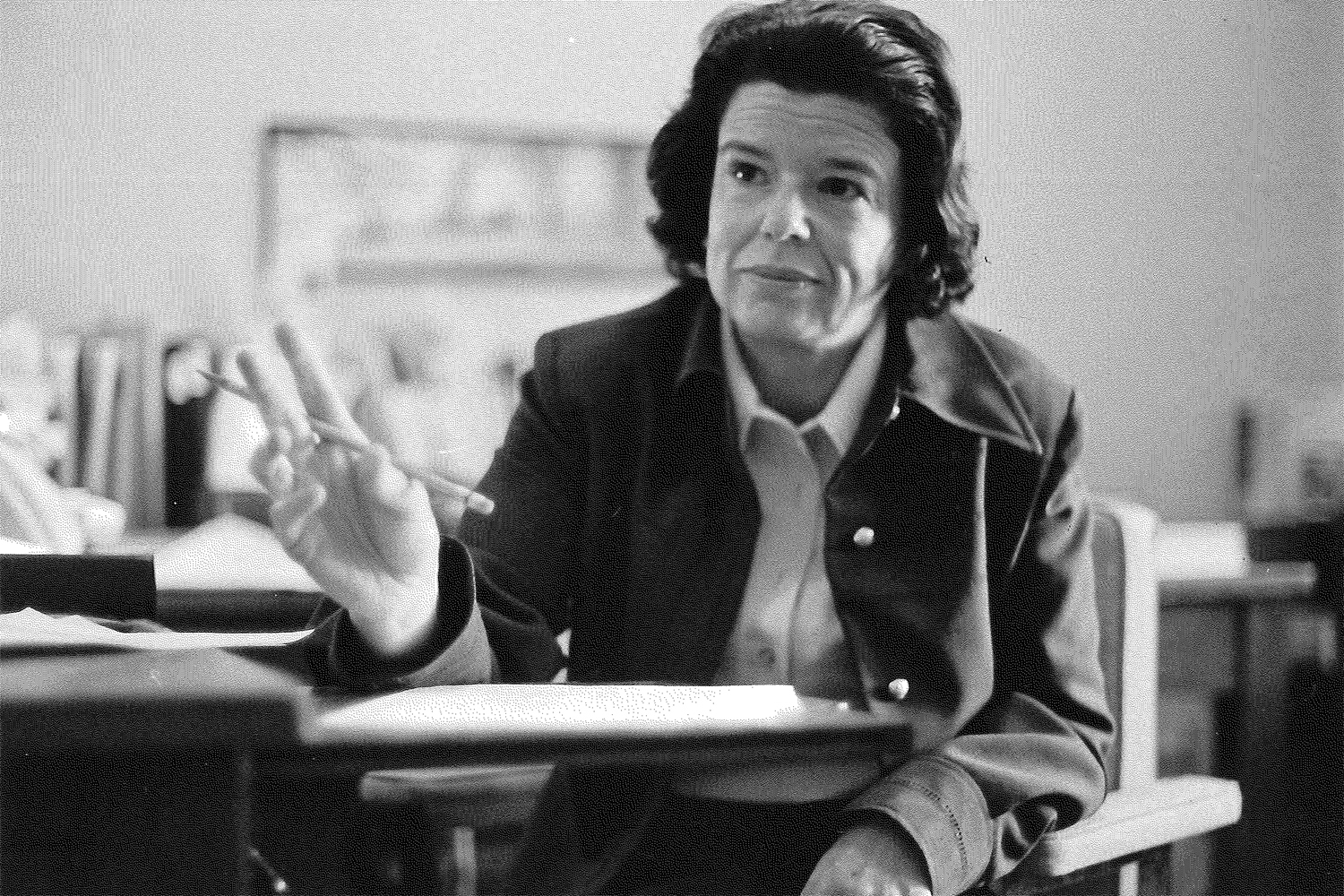
Radolf is leading several research initiatives on Lyme disease in his lab along with associate professor Melissa Caimano and postdoctoral fellow Ashley Groshong in UConn’s Spirochete Research Labs.
From an evolutionary standpoint, humans have nothing to do with B. burgdorferi. The bacteria had adapted to survive in wild animals like mice and ticks. But since ticks are “promiscuous feeders,” meaning they will latch on to and feed from any organism they can, including humans, B. burgdorferi has the opportunity to infect humans.
The reason humans get sick from Borrelia burgdorferi while mice and other hosts don’t is that our immune system is able to identify Borrelia burgdorferi as a foreign pathogen and attacks it. This immune response gives rise to the rashes, headaches, fevers, difficulty concentrating, and fatigue associated with Lyme disease.
One thing that makes B. burgdorferi unique compared to other bacteria is that it doesn’t have a mechanism for synthesizing its own amino acids; instead, it picks up peptides from the host.
“No other bacteria is known to need to use uptake methods to acquire necessary peptides from their host rather than synthesizing them, in some capacity, themselves,” Groshong says.
Groshong is looking at how this system operates and how it could potentially be intercepted by creating blockers that mimic the peptides the bacteria needs that lock onto the sites B. burgdorferi uses to incorporate those peptides.
Another critical component of the enzootic cycle, one that involves bacteria moving between different organisms, is understanding how B. burgdorferi knows in which kind of organism it is.
“It’s important to be able to understand how a bacteria like B. burgdorferi is able to accomplish this remarkable feat of going back and forth,” Radolf says.
Borrelia burgdorferi’s genome is regulated by the rpoS gene which is able to turn the expression of 100 other genes on or off depending on the environment.
This question is the primary focus of Caimano and Radolf’s recent $440,000 NIH grant.
“The spirochete (spiral-shaped bacteria, i.e. B. burgdorferi) has adapted its physiology so it can better compete for nutrients,” Caimano says. “Once the blood meal comes in, the spirochete is competing with the tick itself for nutrients.”
How B. burgdorferi survives in humans, given its need for peptides provided by the host, is particularly perplexing since human tissue is a rather poor source of peptides.
“We don’t think human tissue is flush with peptides,” Groshong says. “It a limited nutritional environment.”
One mystery about Lyme disease that remains unsolved is why some people continue to be sick after they have been treated with antibiotics that kill Borrelia burgdorferi.
The question is whether the bacteria survive in a persistent form that isn’t impacted by the antibiotics or does it somehow change our immune system to leave it in a perpetually symptomatic state?
In the lab, researchers culture bacteria in a nutrient-rich environment that encourages growth, however this doesn’t give researchers a very realistic picture of how the bacteria survive in human tissue.
Groshong is testing if peptide depletion in human tissue gives rise to these persisted cells as a Blackman Fellow of the Global Lyme Alliance.
“If the persistent bacteria exist, their presence can’t be determined by our normal process, so we’re trying to go the long way around and see if they exist,” Groshong says about the research.
B. burgdorferi is a remarkably well-evolved organism and scientists are just beginning to study it.
“Spirochetes have had millions of years to figure this out,” Caimano says. “We’ve only had a few decades.”
But the work being done at UConn Health is certainly making headway into understanding what makes this unique bacteria tick.