Over the past five decades, the HIV/AIDS epidemic has affected millions worldwide. Today 37.9 million people are living with HIV.
Thankfully, there are effective treatments to help those living with HIV/AIDS manage their condition and live a healthy life. However, 21% of people with HIV do not know they have the virus according to 2019 UN AIDS data.
One of the greatest barriers to learning one’s status early is that standard HIV testing methods rely on expensive equipment and well-trained personnel, limiting the availability of testing.
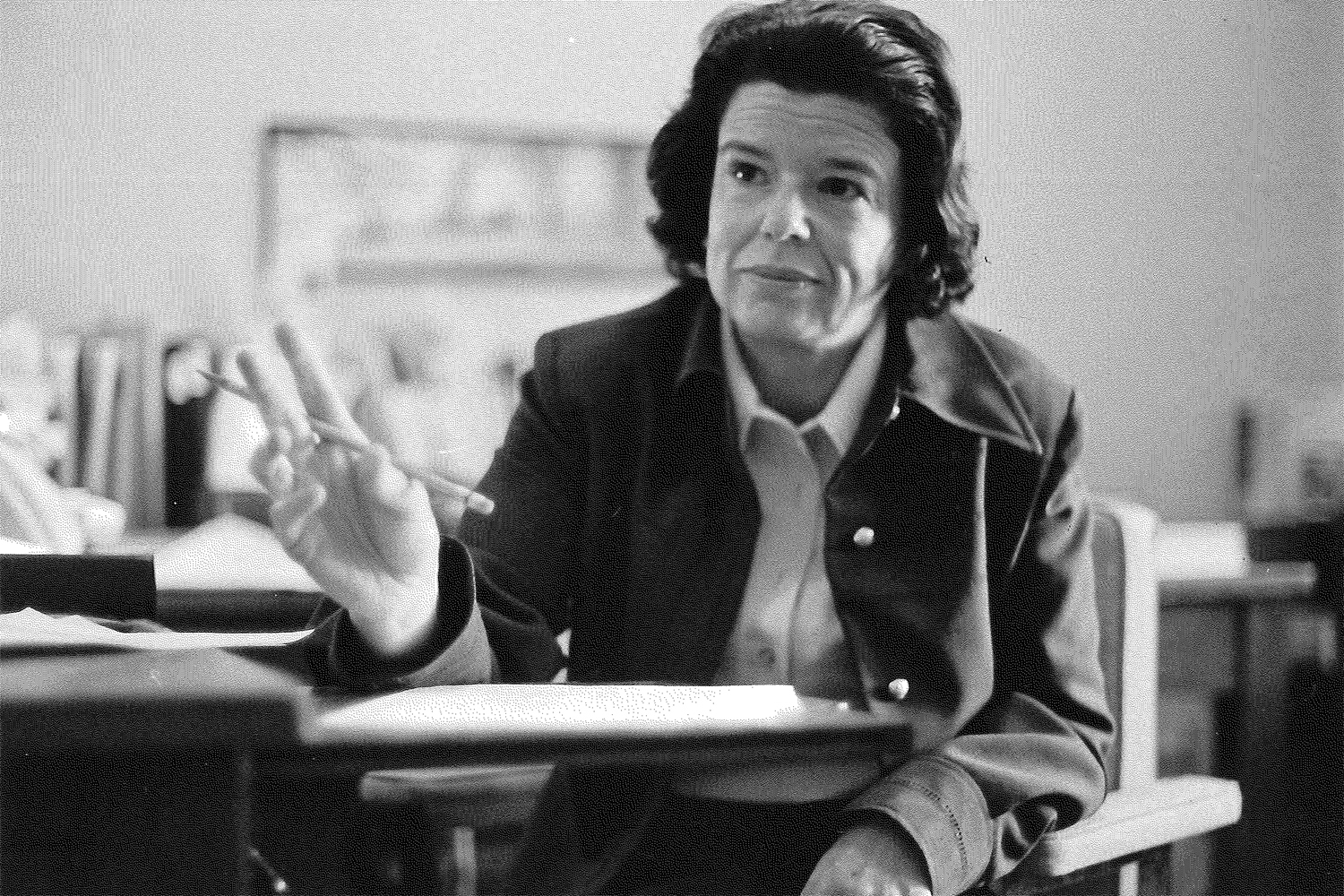
UConn Health professor of biomedical engineering Changchun Liu, Ph.D., has received a $1.4 million grant from the National Institutes of Health to develop a simple, rapid, affordable HIV testing device. Dr. Maroun Sfeir, assistant professor of pathology and laboratory medicine at UConn Health, Dr. David Banach, associate professor of medicine at UConn Health, and Ranjit Warrier, Ph.D., the Director of Central Laboratory at Centre for Infectious Disease Research in Zambia (CIDRZ) are co-investigators on this project.
If HIV spreads within a person’s body unchecked, it may develop into AIDS, which is defined by a set of measures related to the damage HIV inflicts on the immune system. AIDS can make a person more susceptible to a host of illnesses including certain infections and cancers.
Early intervention is essential, as an NIH study found early antiretroviral (ART) treatment lowered the risk of serious AIDS-related events by 72%.
Antiretroviral treatment requires frequent monitoring to confirm treatment effectiveness and identify if the virus is rebounding through viral load testing.
Viral load testing quantifies HIV viral RNA, its genetic material, in plasma. This is a more accurate and reliable approach for acute HIV detection and ART monitoring than antigen and antibody testing.
This invention will diagnose acute HIV infection during the window prior to seroconversion using RNA detection. The seroconversion window is the period during which antibodies develop and during this period an individual may spread infection to others. At the end of this window, HIV antibodies are detectable in the blood. For HIV, this window is up to six weeks after a person is initially exposed.
Commercially available diagnostic technologies rely on testing for HIV antigens and antibodies, making them less effective at detecting acute HIV infections or ART failure.
The lack of an accessible diagnostic tool for HIV RNA detection leaves many individuals unaware of their status, impeding timely ART treatment.
This sensitive platform will be low-cost and take only 35 minutes to produce results. The platform will only require a finger prick volume of blood making it simple and accessible to a great portion of the populations most affected by HIV.
Liu and his team will develop a highly sensitive, specific clustered regularly interspaced short palindromic repeats (CRISPR) biosensing technology for HIV nucleic acid-based molecular diagnostics. The platform will identify viral RNA base sequences specific to HIV.
The next part of their project will be to create a disposable device able to separate plasma from other blood elements, enrich viral RNA to make it easier to detect and apply the CRISPR technology to detect the presence of HIV and assess the viral load.
Liu’s team will evaluate this platform using samples from the United States and Zambia, which have the sixth and seventh highest rates of HIV, respectively, according to 2018 WHO data.
This “blood-to-answer” device will make early at-home HIV detection via RNA accessible and help people begin receiving treatment to manage the virus earlier.
“If successful, such a simple, rapid, affordable detection platform will enable acute HIV diagnosis and viral load testing at home and be appropriate for resource-limited settings where HIV is most prevalent,” Liu says.
Liu holds a Ph.D. in physical electronics from the Institute of Electronics, Chinese Academy of Sciences and a master’s degree in organic chemistry from Yunnan University. His research interests include microfluidic devices, biosensors and bioinstrumentation, wearable technology, medical diagnostics and mobile health.
To learn more about Changchun Liu’s technologies and opportunities to license or partner, contact Amit Kumar, Ph.D. (a.kumar@uconn.edu)