A collaborative effort between the University of Connecticut, Wesleyan University, and The Jackson Laboratory for Genomic Medicine has been contributing a wealth of research to the field of stem cell science since its inception in 2006 during a time when the federal government had instituted a ban on projects using stem cells. The program has received renewed funding of $1 million for the next two years from the Connecticut Bioscience Innovation Fund.
First, here’s a little refresher on what stem cells are and the role they play in human biology. When humans are developing in the womb, they begin as a small bunch of non-differentiated cells – stem cells. As the embryo continues to develop, stem cells gradually turn into specialized cells that make up our various organ systems. Induced pluripotent stem cells, which the Stem Cell Core generates from adult skin, blood, or cells from urine, are reprogrammed back to act as stem cells and have applications in precision medicine and disease models.
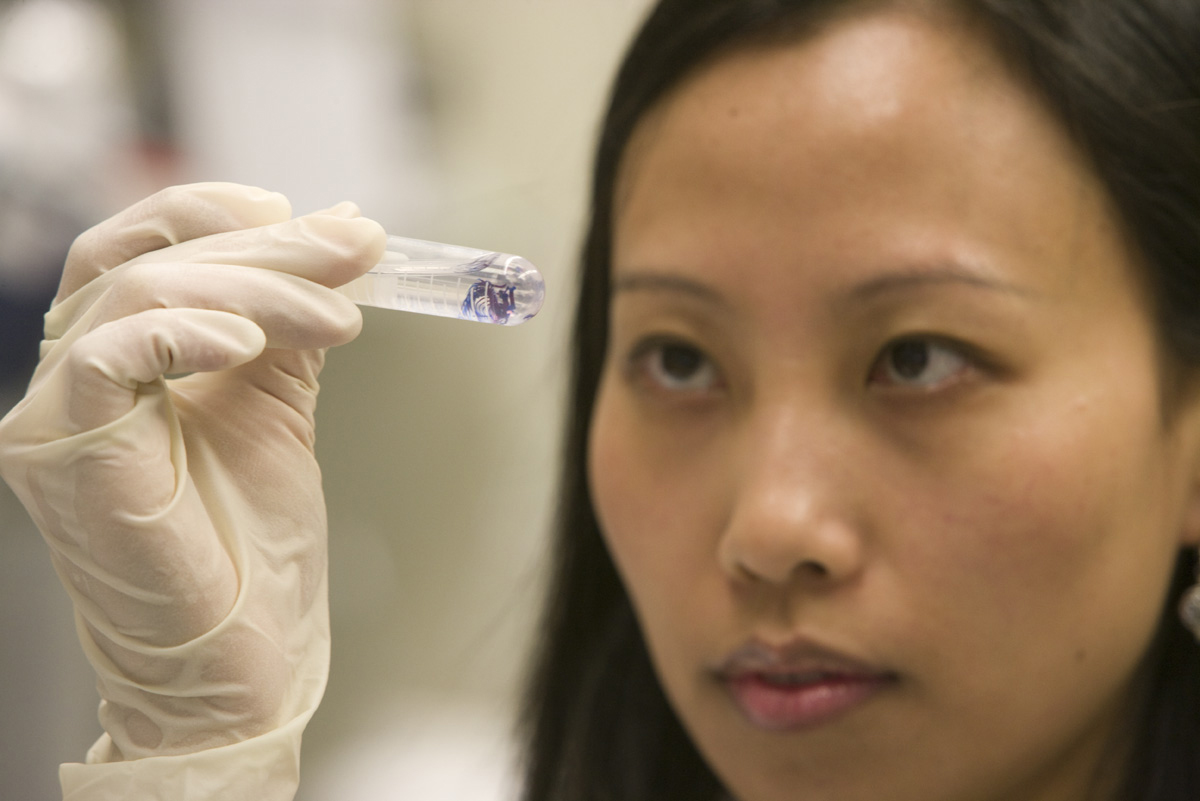
The Stem Cell Core centralizes stem cell research resources and provides training and outreach opportunities for undergraduate and graduate students, as well as the general public. The Core provides genome integrity analyses, stem cell training and quality control services and reagents.
“When researchers publish papers using their own stem cell lines, the expectation from the scientific community is that they will share their resources,” Leann Crandall, lab manager of the Stem Cell Core says. “But if the receiving party doesn’t know how to use them, they can’t get the work done. The work we do in the Stem Cell Core helps train researchers to be able to utilize stem cells to further the field,” she says.
The Core’s location on the UConn Health Campus provides a direct pipeline to experts in different fields.
“The nice thing about being at UConn Health is that we have specialists in every major tissue type right here,” Gordon Carmichael, principal investigator of the grant and UConn Health professor of genetics and genome sciences says.
Carmichael says the work he and his former graduate student, Ling Ling Chen, who is now an accomplished scientist working in China, did on RNA molecules turned out to be closely related to the work of another Stem Cell Core researcher.
“The Stem Cell Center was absolutely integral,” Carmichael says. “We couldn’t have done our work without the stem cell models.”
The Stem Cell Core has given rise to four NIH-approved lines of human embryonic stem cells to serve as the basis for applications research. It has also generated induced pluripotent stem cells, which come from adult cells that are reprogrammed back to act as stem cells, for 80 labs at UConn and other institutions in the state. The program was also instrumental in the launching of two university-based stem cell companies, ImStem and Chondrogenics.
Currently, the Stem Cell Core is developing a biobank of tissue from UConn Health patients. This will allow an individual’s genome to be linked to their health data which can be used in future precision medicine studies by generating stem cells from a person’s own tissue.
“We can probe exactly what’s causing this disease at a level never before possible because we have the stem cells and new biochemical methods,” Carmichael says.
Stefan Pinter, a UConn Health assistant professor of genetics and genome sciences has used both the stem cell core and the UConn Center for Genome Innovation for his research on Turner syndrome, in which a female only has one X chromosome, and Down syndrome which is caused by the presence of an extra 21st chromosome.
“I don’t think I would have chosen these two areas if we didn’t have such an excellent stem cell core in house,” Pinter says. “We need a larger number of iPSC colonies to screen early on, when their cell numbers are still small, which presents a logistical challenge.”
The core helped Pinter get four times the standard number of induced pluripotent stem cell colonies for his research which requires being able to see which colonies have the right number of chromosomes and which ones lack a chromosome or have one extra, as is the case in Turner’s and Down’s.
“We wouldn’t have been able to do this research without the core. We wouldn’t have had enough time and enough experience to do the research,” says Pinter. “It made a huge difference.”
Chris Heinen, UConn Health associate professor of medicine in the Center for Molecular Oncology, has used a human pluripotent stem cell line at the Stem Cell Core as a model for his research on Lynch syndrome, a hereditary condition that makes individuals predisposed to certain kinds of cancer.
“We like human pluripotent stem cells as a model cell because it’s a human cell line that’s immortal and is not a cancer already,” Heinen says.
Heinen says the Stem Cell Core has been instrumental in driving his work forward. He credits the Core with helping him win several grants for which he otherwise would have been out of reach.
“The core serves as a source of information, new ideas, and new technology we can then adapt to our own work,” Heinen says. “Our work would not have been able to go in the direction it did without the core.”
This renewed funding will allow the Stem Cell Core to maintain its first-in-class status as a technical and training resource for stem cell research in Connecticut.
“We keep going as the science keeps going,” Crandall says. “We’re moving pretty quickly along with the science.”