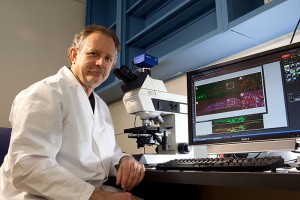
Whether it’s an older adult who is suffering from osteoporosis, a soldier who has lost a limb, or a child born with a debilitating bone disorder … all may eventually benefit from the research being done in the lab of Alexander Lichtler in the Department of Reconstructive Sciences at the UConn Health Center.
Lichtler’s goal is to develop improved methods of changing stem cells into cells that can repair bones. “The reason that we want to do this is because the currently available methods for producing these cell types are generally not very efficient,” he says.
Lichtler first received state stem cell funding in 2006, the first year grants were awarded by the Connecticut Stem Cell Research Advisory Committee. His project was one of nine comprising the University’s group project grant, Directing hES Derived Progenitor Cells into Musculoskeletal Lineages, headed by David Rowe and totaling $3.5 million.
“Sometimes I like to say that the good thing about embryonic stem cells is that they can become any cells in the body and the bad thing about embryonic stem cells is that they can become any cells in the body,” says Lichtler. “We want to be able to push them in the direction we want them to go, and not let them do whatever they want to do.”
That’s why Lichtler and fellow researchers David Rowe, Ivo Kalajzic, and Peter Maye are focusing on deciphering the stages of bone cell development and how to control it.
“I know most about bone but there are different types of bone cells … a skull bone is quite different than a long bone, a femur,” Lichtler says. “So let’s say a soldier sustained a head injury, you want to repair his skull with bone cells that will differentiate into a skull, not a leg bone.”
Currently, scientists don’t have accurate markers that show whether the cells you’re seeing in the petri dish will eventually end up as leg, skull, or back bone.
“One of the first steps in becoming a bone, cartilage, skin, or muscle cell is to become a mesoderm cell,” Lichtler says, “and one of our main goals is to develop ways to easily detect when a human embryonic stem cell has differentiated into a mesoderm cell.”
Part of the group’s research involves producing embryonic stem cells equipped with fluorescent protein markers that “come on” when the cells have reached a certain differentiation stage. This will help them better determine whether the cells will become leg, skull, or back bones.
This year Lichtler and Ernst Reichenberger, a fellow researcher in the Department of Reconstructive Sciences, were awarded an Established Investigator Grant from the state for $500,000. Their research zeroes in on a specific bone disorder – craniometaphyseal dysplasia. CMD is a rare and debilitating bone disease with sometimes fatal overgrowth of skull bones. It affects children and progresses throughout their life. There is currently no treatment.
The researchers hope to obtain skin biopsies from CMD patients and compare them with normal skin cells to better understand how a gene mutation causes them to be different. They will first convert them into induced pluripotent stem cells, or iPSC, which are very similar to embryonic stem cells, and then convert them into the types of bone cells that are defective in CMD patients before doing the analysis.
“In basic science, you never know what discovery will have some relevance to treatment,” says Lichtler. “There’s always a chance you’ll learn something, some new concept of why this particular gene causes a mutation, and it may lead you to a new therapy. That’s what we’re hoping for.”