It’s common to hear complaints about our near-constant connection to our smart phones, but UConn researchers believe they can use the ubiquity of these devices to better screen for depression.
Depression is an affliction that affects 350 million people worldwide, and one of the most crucial issues for mental health workers is detecting it in patients in its early stages. Bing Wang, associate professor of computer science and engineering, says smartphones have the potential to serve as “human sensors” by monitoring users in real time for symptoms of depression.
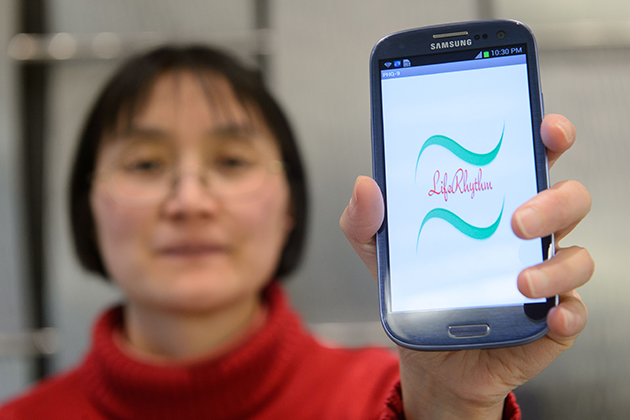
Wang, who joined the School of Engineering in 2005, has developed a mobile phone app, LifeRhythm, which gathers data from various sensors on the phone – location, motion, microphone, among them. The project is funded with a $718,815 grant from the National Science Foundation Directorate for Computer and Information Sciences and Engineering. She’s working on it with Jinbo Bi and Alexander Russell in the Department of Computer Science & Engineering at UConn, Dr. Jayesh Kamath, associate professor of psychiatry and immunology at UConn Health, and Nasos Bamis, a consultant to this project.
Wang says there are certain behavior signs, such as activity, energy levels, and social interactions, that can be inferred from the data collected by a smartphone’s many sensors. GPS, for instance, gives us information about how often and how far people venture outside their homes. Sound sensors pick up on certain features of the user’s speech; studies have shown that simple acoustic features such as tone, the duration of pauses, and loudness are useful for detecting depression. Accelerometers and gyro sensors provide hints on the physiological activities and energy level of a user. And the number of phone calls and SMS messages that a user initiates and receives indicate his/her interest in interacting with other people.
If the technology of LifeRhythm were widely adopted, it would revolutionize how depression is diagnosed. Because there are no direct biomarkers to diagnose depression in common clinical practice, various interview-based methods have been developed to screen for depression. The most commonly used test is the Patient Health Questionnaire-9 (PHQ-9) developed in 1999. The nine criteria it screens for are anhedonia (inability to experience pleasure), depressed mood, trouble sleeping, fatigue, change in appetite, feelings of guilt or worthlessness, trouble concentrating, feeling slowed down or restless, and suicidal thoughts.
These questionnaires are considered reliable screening tests, Wang says, but they have their shortcomings. For one, it takes time to fill them out on a regular basis – and those suffering from depression may not want to take that time. In addition, patients have to rely on their memory to fill in the questionnaires, or their answers may be biased toward what they think clinicians want to see. Another drawback is that there is a shortage of clinicians trained to specifically administer and interpret the questionnaires. By contrast, the LifeRhythm app collects the data automatically, and the information is objective.
They hope to recruit 120 student subjects for the first phase of the study, which will last for one semester. Half of the group would have a prior history or current symptoms of depression and the other half would not. For the second phase, they plan to recruit 300 students. During this phase, the researchers will refine the data collection process.
“We will only focus on students living on campus,” Wang said. “College students are more likely than others to be depressed – they’re very young, away from home for the first time, and there’s all kinds of stress.”
Wang says the study could be the first step in dealing with depression in mass populations, and help mental health workers identify depression promptly. It could also contribute significantly to public health by raising awareness about depression. In the future, she adds, the technology could be enhanced to take a more active role in treating patients with various intervention techniques.
“The intervention could be as simple as a text saying ‘Go out for a walk,’” she says. “Intervention would be a very natural next step.”


