One of the drawbacks of chemotherapy is that cancer patients can build up resistance to treatment over time, increasing their chances of possible relapse.
Finding a way to suppress that resistance would be a major step toward boosting the therapeutic effects of some cancer-fighting drugs.
UConn medicinal chemist M. Kyle Hadden, working in collaboration with UConn Health molecular biologist Dmitry Korzhnev, has identified several small molecules that disrupt the ability of certain cancer cells to bypass the damage caused by chemotherapy, a key component in the onset of resistance.
These molecules could serve as the foundation for a new drug that could be delivered in combination with anti-cancer medication to make long-term chemotherapy treatments more effective.
While the findings are encouraging, Hadden cautions that the discovery is an initial step and that new drug development is a lengthy process that can take 10 years or more. Much more laboratory and clinical research needs to be done, he says, before a potential drug could be put into use.
“What we’re trying to do is develop a drug that can be given at the same time as an anti-cancer agent, so the pair work together to make sure that cancer cells die during chemotherapy treatment and aren’t rescued,” says Hadden, an associate professor in the Department of Pharmaceutical Sciences.
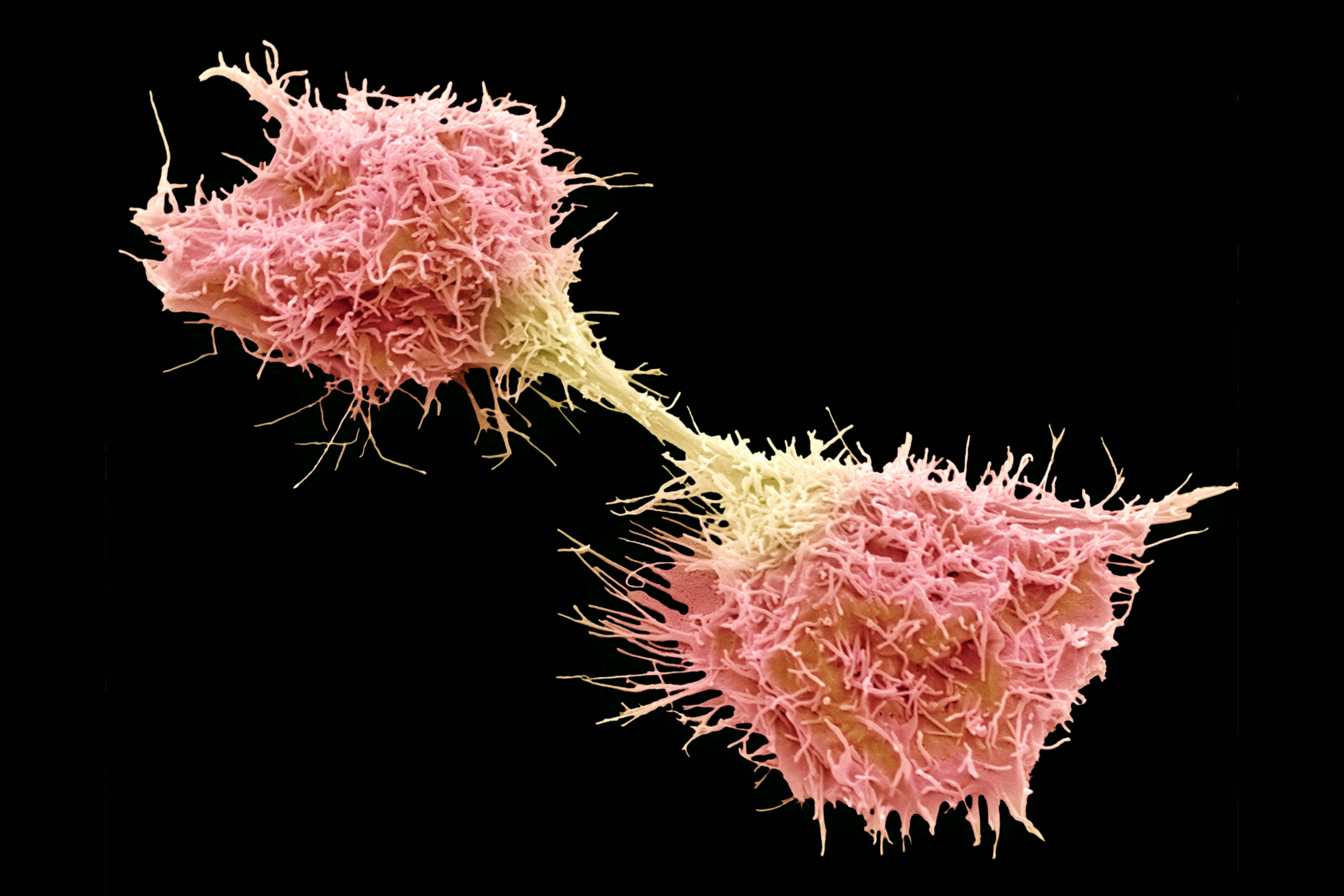
In identifying the molecules, Hadden’s lab studied fibrosacrcoma cancer cells that were treated with cisplatin, a leading platinum-based anti-cancer agent also known by the commercial trade name Platinol. Cisplatin causes DNA damage in cancer cells, which hinders the cells’ ability to copy their genomes and multiply, essentially killing them.
But all cells, including cancer cells, have a way of thwarting death by activating a process known as translesion synthesis or TLS. When a cell detects DNA damage, it calls the TLS process into action. TLS acts like a fixer, a cellular mechanic you might say, that rescues the cell by releasing enzymes that allow the cell to bypass damaged DNA and continue dividing and multiplying. The TLS process is far from perfect, however. Many of the new cells that are created have mutations that increase the presence of cancer and lead to rapid growth of drug-resistant cells.
In order to stop cancer cells from building up resistance, Hadden and Korzhnev knew they had to disrupt TLS and keep the fixer at bay. Korzhnev’s lab was instrumental in identifying key protein interactions that take place during the TLS rescue process and where they were happening inside the cell. One protein in particular, a Y-family polymerase known as Rev1, appeared to orchestrate the alignment and binding of proteins to carry out the rescue effort. On top of that, Korzhnev, an expert in nuclear magnetic resonance spectroscopy, isolated a small portion of the Rev1 protein structure – an area known as the C-terminal domain – as being a critical junction for the process to work.
Armed with that information, Hadden ran more than 10,000 compounds through an intricately designed high-throughput screening assay to see if any of them disrupted the protein interactions taking place in Rev1 at the C-terminal domain. Two small molecules – thiophenes and piperazines – emerged as having the chemical and structural properties needed to throw a wrench into the TLS works and disrupt the process.
“Ideally, what we are hoping to show is that if you dose the cells with our TLS inhibitor and dose them at the same time with cisplatin, you get the same effect of killing cancer cells and you can achieve that effect with a smaller dose of cisplatin,” Hadden says. “This would ideally combat resistance and reduce the need for high doses of cisplatin and the associated side effects.”
In a recent paper published in the peer review journal Bioorganic & Medicinal Chemistry, Hadden reports that with additional research he has now identified as many as five molecules that could be considered for stopping TLS.
“We’ve really expanded the number of compounds that do this and that could be put forward as potential drugs,” Hadden says. “This is good, because one of the challenges of drug discovery is that if you only have one compound to work with and something bad happens down the line, then you can have a problem. This way, we can focus on a few of the molecules, but we also know we have backups if those don’t work.”
With the help of UConn’s Technology Commercialization Services, Hadden and Korzhnev have applied for a provisional patent for the discoveries. They are also conducting further research in an effort to better understand how the molecules interrupt the TLS process and whether, over time, they will indeed hinder chemotherapy resistance in cancer cells.
The research team is looking to apply what it has learned about TLS to other cancers as well, such as non-small cell lung cancer and ovarian cancer.
Korzhnev and Hadden are already exploring ways to optimize the molecules’ performance.
“Optimization of lead compounds requires aspects of medicinal chemistry but also structural information to guide the process,” says Korzhnev, an assistant professor in the Department of Molecular Biology and Biophysics at UConn Health. “So we not only need development of the molecules, but also we need to know what they do in cells, and that’s where my lab can help.”
Zuleyha Ozen, a former research technician in Hadden’s lab, performed all of the compound screening work and serves as first author on the paper published in Bioorganic & Medicinal Chemistry. Radha Dash, a postdoctoral fellow in the Hadden lab, provided the paper’s computational modeling data.
For one member of the research team, UConn sophomore Samantha Chow, the TLS project has been a thrilling experience. Chow joined the team as a Glastonbury High School senior as part of a program called, Advanced Research Mentorship or ARM. The program links students to professional researchers in their field of choice. As a member of Hadden’s lab, Chow helped Ozen screen potential compounds. Chow, now a pre-pharmacy major at UConn, continues to work in the lab.
“I was able to learn skills I never could have as a high school student,” says Chow. “I not only gained valuable lab skills, but I also learned how to analyze data. It never occurred to me that the work I was doing – the screening, the dilutions, the cell cultures – would be an integral part of this project. To be listed as a co-author on the final published research article is a great honor.”
This research was supported by National Science Foundation grant #1615866, the University of Connecticut Research Foundation, and the Connecticut Institute for Clinical and Translational Sciences.