Memory loss, confusion, misplacing things – these are all familiar symptoms of Alzheimer’s disease. However, there is actually a more common sign that often goes undetected: apathy.
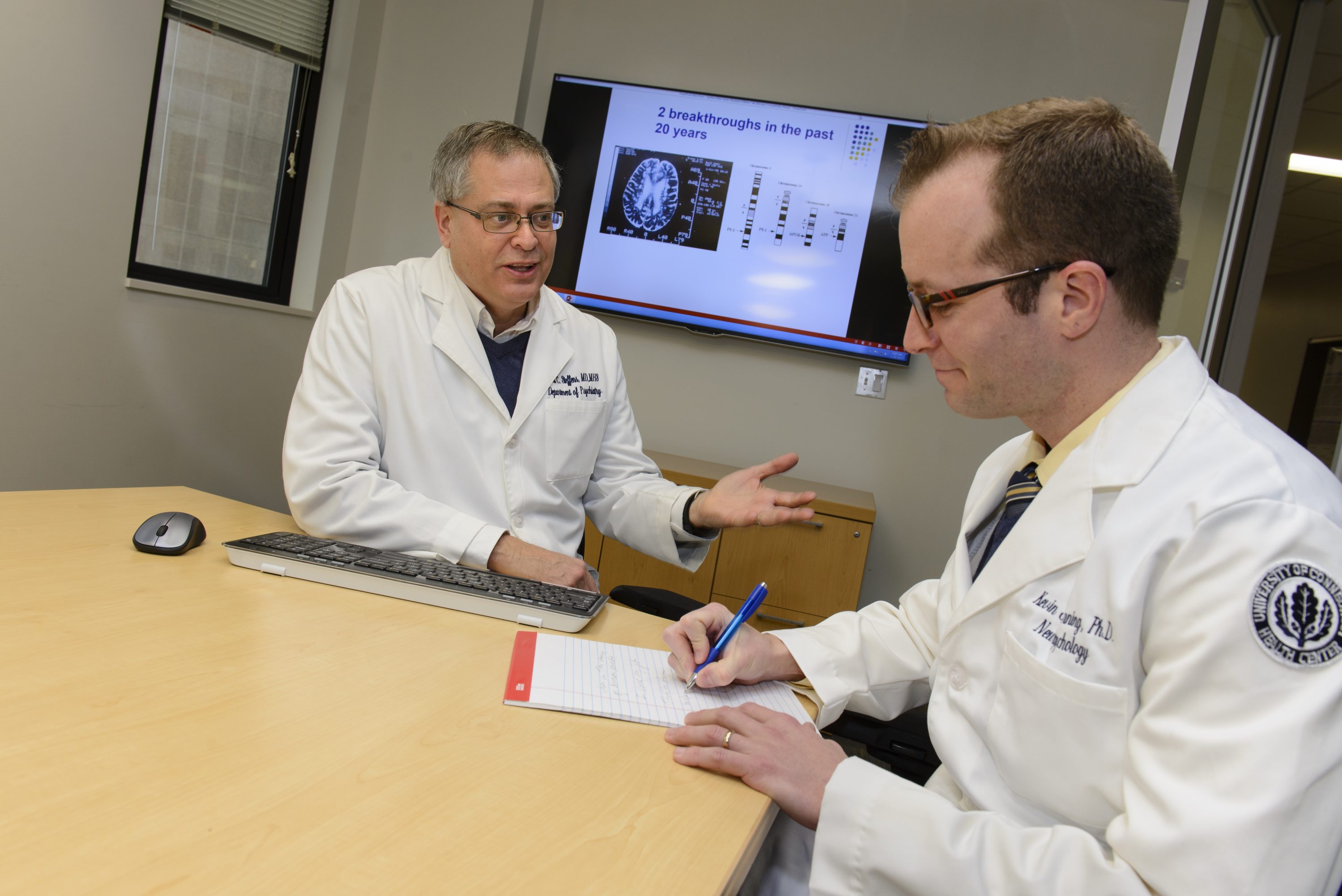
Chair of psychiatry in UConn’s School of Medicine, Dr. David Steffens, is conducting research on apathy; the most common neuropsychiatric symptom in patients with Alzheimer’s disease. Along with co-investigators at UConn Health, Steffens received a $451,000, two-year award from the National Institute of Mental Health.
Traditionally, apathy has been defined as a loss of motivation in at least two of the three domains: goal directed behavior, cognitive activity, or emotion. In Alzheimer’s disease, apathy has also been related to caregiver distress, decreased quality of life, and increased morbidity. While its effects are clearly problematic, the underlying neurobiology of apathy is poorly understood and brain networks that contribute to clinical apathy are unclear.
Recently, apathy syndromes have been tied to brain-based Positive Valence Systems, which are responsible for responses to positive situations. These systems include reward evaluation, including anticipation of reward and reward sensitivity, along with willingness to work and how one makes a judgement based on whether to act on obtaining a reward.
Steffens proposes to link a Positive Valence Systems approach with clinical measures of apathy and with functional imaging to better understand apathy regarding Alzheimer’s. Steffens’ and the UConn Health research team will look at how Alzheimer’s-associated apathy differs from apathy in people diagnosed with late-life major depression. Steffens’ research will use functional magnetic imaging (fMRI) and tasks that focus on the brain’s reward system to examine apathy in Alzheimer’s and in late-life depression.
Steffens plans to examine neurocognitive and neurobiological differences in patients with Alzheimer’s disease and late-life major depression. Along with that, they will look at the similarities and differences in clinical and neuropsychological characteristics and neurobiological features of apathy across these conditions.
This research will help to identify new targets for intervention to improve apathy in patients with Alzheimer’s and will also further knowledge regarding differences in reward-based neurobiology. More specifically, Steffens hopes to show how apathy differs both clinically and neurally between Alzheimer’s and late-life major depression.
Co-investigators from UConn’s School of Medicine include Grace Chan, Kevin Manning, and Lihong Wang.
Dr. David Steffens, MD, MHS is chair of the Division of Psychiatry in UConn’s School of Medicine. He is a past president of the American Association for Geriatric Psychiatry and has written more than 300 peer-reviewed papers. Steffens is an associate editor of the American Journal of Geriatric Psychiatry and his interests lie in late-life depression and cognitive disorders in older adults. For over 25 years, Steffens has been funded by the National Institute of Mental Health and the National Institutes of Health. His research has also been supported by a generous gift from the Leo and Anne Albert Trust. Additionally, working with colleagues in the Department of Psychiatry and the UConn Center on Aging, he developed a clinical geriatric mental health service that focuses on assessment and treatment of anxiety, depression and cognitive disorders in the elderly.
NIH Grant #1R21MH120698-01