Biomedical engineers at the UConn School of Dental Medicine recently developed a handheld 3D bioprinter that could revolutionize the way musculoskeletal surgical procedures are performed.
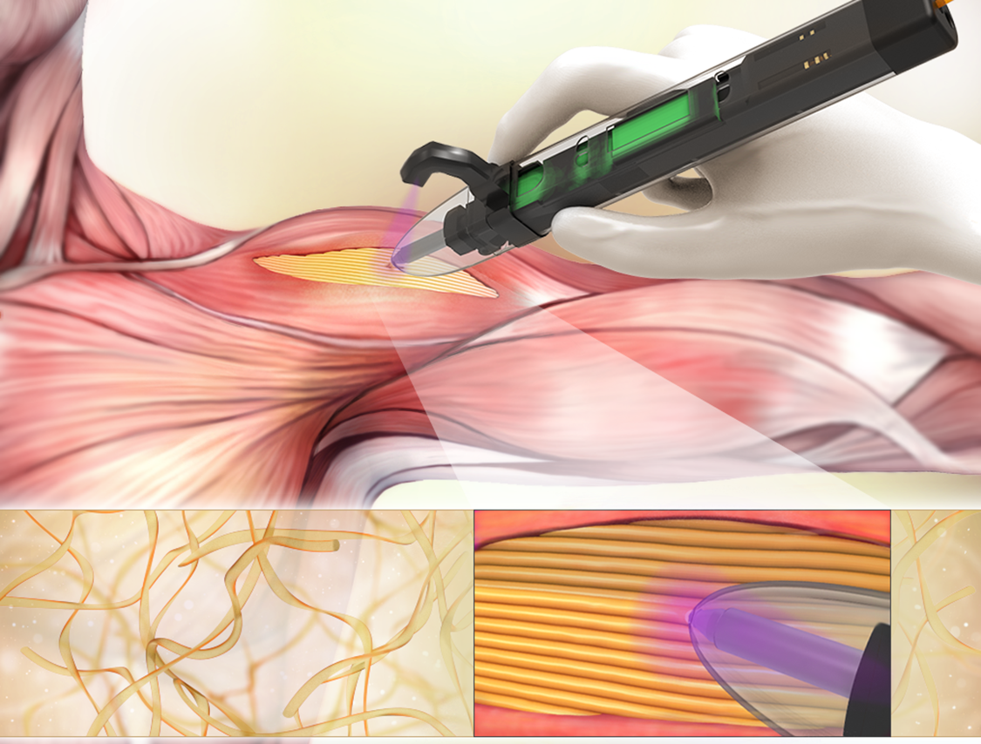
The bioprinter, developed by Dr. Ali Tamayol, associate professor in the School of Dental Medicine biomedical engineering department, enables surgeons to deposit scaffolds—or materials to help support cellular and tissue growth—directly into the defect sites within weakened skeletal muscles.
Tamayol’s research was recently published in the American Chemical Society journal.
“The printer is robust and allows proper filling of the cavity with fibrillar scaffolds in which fibers resemble the architecture of the native tissue,” says Tamayol.
The scaffolds from the bioprinter adhere precisely to the surrounding tissues of the injury and mimic the properties of the existing tissue— eliminating the need for any suturing.
Current methods for reconstructive surgery have been largely inadequate in treating volumetric muscle loss. As a result, 3D printing technology has emerged as an up and coming solution to help reconstruct muscle.
Dr. Indranil Sinha, a plastic surgeon at Brigham and Women’s Hospital at Harvard joined Tamayol in this research study. With expertise in treatment of muscle injuries, Sinha says that a “good solution currently does not exist for patients who suffer volumetric muscle loss. A customizable, printed gel establishes the foundation for a new treatment paradigm can improve the care of our trauma patients.”
Existing 3D bioprinting technology is not without its problems. Implanting the hydrogel-based scaffolds successfully requires a very specific biomaterial to be printed that will adhere to the defect site. While 3D bioprinted scaffolds mimicking skeletal muscles have been created in vitro, they have not been successfully used on an actual subject.
Tamayol’s solution fixes the problem. Tamayol’s bioprinter prints gelatin-based hydrogels – known as “bioink”—that have been proven to be effective in adhering to defect sites of mice with volumetric muscle loss injury. The mice showed a significant increase in muscle hypertrophy following Tamayol’s therapy.
“This is a new generation of 3D printers than enables clinicians to directly print the scaffold within the patient’s body,” said Tamayol. “Best of all, this system does not require the presence of sophisticated imaging and printing systems.”
Tamayol and Sinha have filed a patent on this technology for the treatment of musculoskeletal injuries.
Tamayol also recently developed a “smart bandage” to help clinical care for people with chronic wounds.
This research has been funded by National Institutes of Health and The Gillian Reny Stepping Strong Center for Trauma Innovation.