Faculty from the Division of Endodontology and Department of Biomedical Engineering at the UConn School of Dental Medicine recently received a total award of $462,964 from the National Institutes of Dental and Craniofacial Research (NIDCR) to test a novel way to quantify tooth pain and to develop a patient-friendly smartphone sensor to measure it.
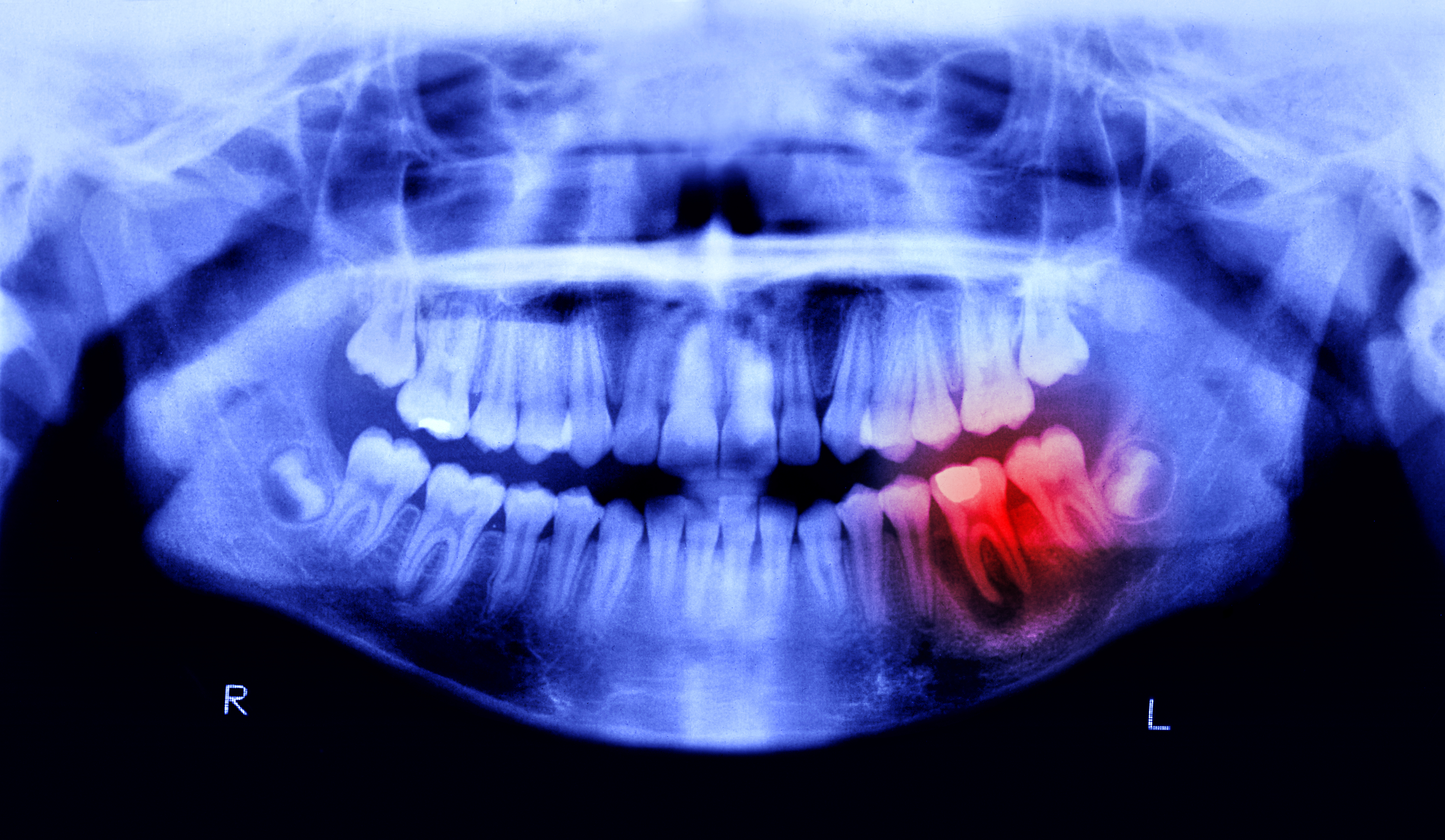
Dr. I-Ping Chen, associate professor of endodontics, and Dr. Ki Chon, professor and chair of biomedical engineering, collaborated on the grant proposal. As an endodontist, Chen cares for patients in need of a root canal. However, Chen and her colleagues heavily rely on a patient’s subjective opinion to gauge the patient’s level of pain. Dr. Chen was looking for a better way to detect dental pain.
“Relying on patient response, which is more subjective, can be problematic, especially when patients can’t communicate with their providers—like children, disabled patients, and patients with language barriers,” says Chen.
Chen learned that Chon had used a commercially available device in his lab that can detect the activity of the sympathetic nervous system, the way the body registers pain. The device is currently used to detect the conductivity of skin, which has the potential to reflect the effects of changes in pain level on a patient. Using this quantitative measurement for dental diagnosis and dental pain detection is a novel concept.
“I knew Ki had this device, and I was looking for something to measure tooth ache. After talking to Ki, we thought we could actually use this in dental patients,” says Chen, identifying one aim of the joint grant proposal.
There is one problem, though. Chon’s device is the size of a laptop.
“The device is already commercially available,” Chon says. “The problem is that we have to miniaturize it,” which is the other aim of the NIH proposal.
With the grant money, Chon will work on a small, smartphone-based sensor and application that works with the electrodermal device. In the meantime, Chon will work alongside Chen to test it on patients, collect data, and determine if the smartphone sensor is an effective and reliable device. The project will take place over the next two years.
If all goes well, Chen and Chon hope that this device can be used by both providers and their patients in dental offices to get a more accurate, quantitative measurement of patient pain, and be able to provide care accordingly.
“For the future, if this can be a validated diagnostic tool, I would imagine that providers would get this device,” says Chen. “I think the long-term goal is that patients can use their smartphone, and they would just download the app and measure pain from home. They would send the result back to their dentist and their dentist would assign the right painkiller.”
“The innovation is the analysis that we have, and how we process the data and measure pain quantitatively,” says Chon. “That’s the potential.”
This project is supported by Grant R21DE029563 from the National Institute of Dental and Craniofacial Research (NIDCR).