Babies who are born prematurely have to fight through days, weeks, or even months of stressful existence.
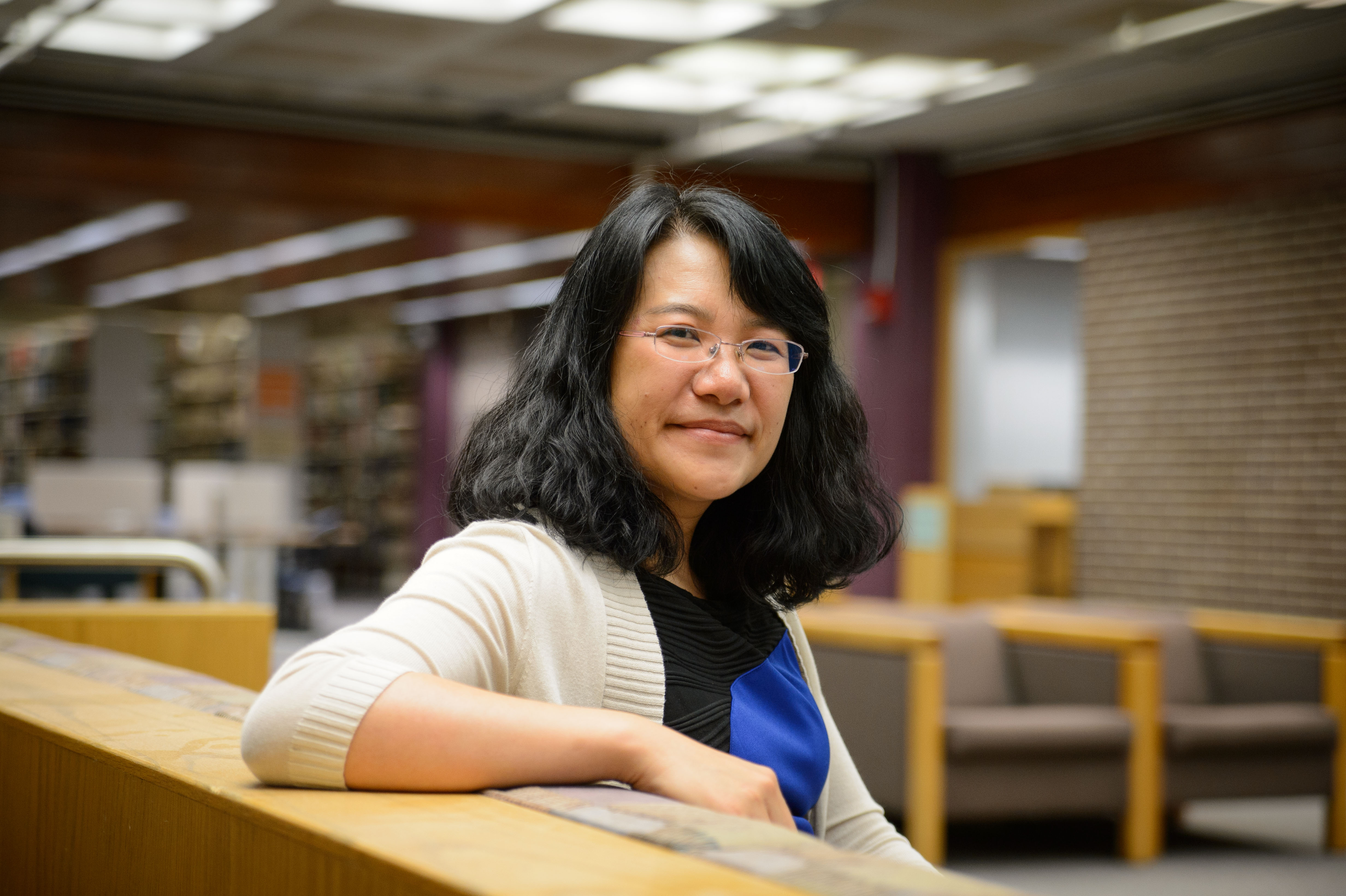
University of Connecticut School of Nursing professor Xiaomei Cong saw this struggle firsthand working as a registered nurse in a neonatal intensive care unit (NICU) early in her career. She watched as these vulnerable newborns underwent up to 20 painful procedures a day. She had always been a practitioner, but these experiences pointed her towards providing support through research and innovation.
These stressful events can have long-term neurobehavioral effects. These effects are one of the focuses of Cong’s research.
One of Cong’s earlier studies focused on how “Kangaroo Care” – a method of holding newborns – can alleviate NICU procedural pain. Kangaroo Care involves skin-to-skin contact, an important aspect for any baby’s development. Cong found for neonates undergoing painful procedures, this has an added benefit of alleviating some of the pain and stress that those procedures induce.
Cong also studies longer-term effects of these stressful events early in life. Focusing on children from birth to three years old, Cong looks at their language development, weight, height, emotional development, cognition and how these children respond to stressful events.
Much of Cong’s current research focuses on using biomarkers to measure stress in babies. Neonates cannot express when they are experiencing stress or pain in the same way older children can. Cong has thus looked to biomarkers like cortisol, a stress hormone and oxytocin, a “love hormone or cuddle chemical” in neonates’ saliva. These chemicals can tell researchers and clinicians a lot about how a baby is handling stress without words.
What’s in the gut
Cong’s research has recently pivoted to look at neonates’ microbiome. The microbiome is a dynamic system of bacteria, microbes, and other organisms that live in and on the human body. The organisms in the microbiome outnumber cells in a human body by approximately 10 to one.
The microbiome supports important digestion, immunity, and nutrition functions. A person accumulates their unique microbiome over their lifetime. Babies are born as a clean slate and begin growing their biome right from birth. The first few months of life are key to developing a healthy biome for the rest of a person’s life.
“They undergo big changes in those first few weeks of life,” Cong says.
When babies are in the NICU, they are not exposed to the normal bacteria and microbes because their health is so fragile.
One of Cong’s current studies looks at mothers who are unable to breastfeed their infants in the NICU. Often, these babies will be tube-fed pasteurized breastmilk from donors. Compared to mother’s own milk, this milk may have disadvantages, because pasteurization kills many of the helpful bacteria and microbes along with those which may endanger the babies’ nascent immune systems.
“It has the same nutritional value, but hampers the development of the microbiome,” Cong says.
Cong has found that milk from the baby’s own mother, even if it has to be through tube-feeding for the very premature infant, is better for the baby’s microbiome development than that of pasteurized donor milk.
This finding helps inform clinical practice, as doctors and nurses can encourage mothers to send their own milk to the NICU even when they cannot breastfeed directly.
Cong also studies stool samples from neonates to look for additional biomarkers that reveal the development and health of their microbiome, as well as the microbiome of people with Irritable Bowel Syndrome (IBS). Cong is studying the manifestations of emotional stress in patients with IBS using many of the same concepts she uses to study neonates in the NICU.
Keeping up with tech
More recently, Cong has also used genetic markers to study this aspect of neonates’ experience in the NICU. The emergence of genomic science has provided a new avenue for Cong to expand her research.
“We always have these new technologies,” Cong says. “Especially in recent years with genetics and genome science, we really have to catch up with what’s going on there.”
These advancements have shown Cong how important fruitful collaborations with other researchers can be. Cong works with researchers at Connecticut Children’s Medical Center and The Jackson Laboratory for Genomic Medicine, who have expertise in areas that can inform her research.
“You always have to learn some new thing,” Cong says. “And that often means you have to build up your team and work together.”
Cong also works closely with the Microbial Analysis, Resources and Services (MARS) center, which is part of UConn’s Center for Open Research Resources and Equipment (COR2E), which conducts microbiome sequencing. Cong is also the director of the UConn School of Nursing’s Biobehavioral Research Lab.
“All the collaborations are so important to our studies,” Cong says. “We get amazing results.”
Not just on paper
One of the most rewarding aspects of her work for Cong is how directly it can be applied and have real-life impacts.
“It goes into clinical practice,” Cong says. “It’s not just on the paper.”
The goal of Cong’s research is to improve the short- and long-term neurodevelopment and quality of life for babies who start their lives in the NICU.
Cong says she sees her research continuing in new directions facilitated by technological developments which support new avenues for her work.
“Definitely we want to see all these babies have an improved quality of life and better health later in life,” Cong says.