Neurodegenerative diseases affect millions of people worldwide. Associated with a combination of age-related changes, genetic and environmental factors, scientists are still grappling with the exact causes of these diseases.
While most research on the causes and contributing factors of neurodegenerative diseases have focused on neurons and other cells within the brain, a team of UConn Health researchers will pivot the conversation to look at another important factor: age and dementia-linked changes in the endothelial cells composing the “blood-brain barrier” in the vasculature that feeds the brain.
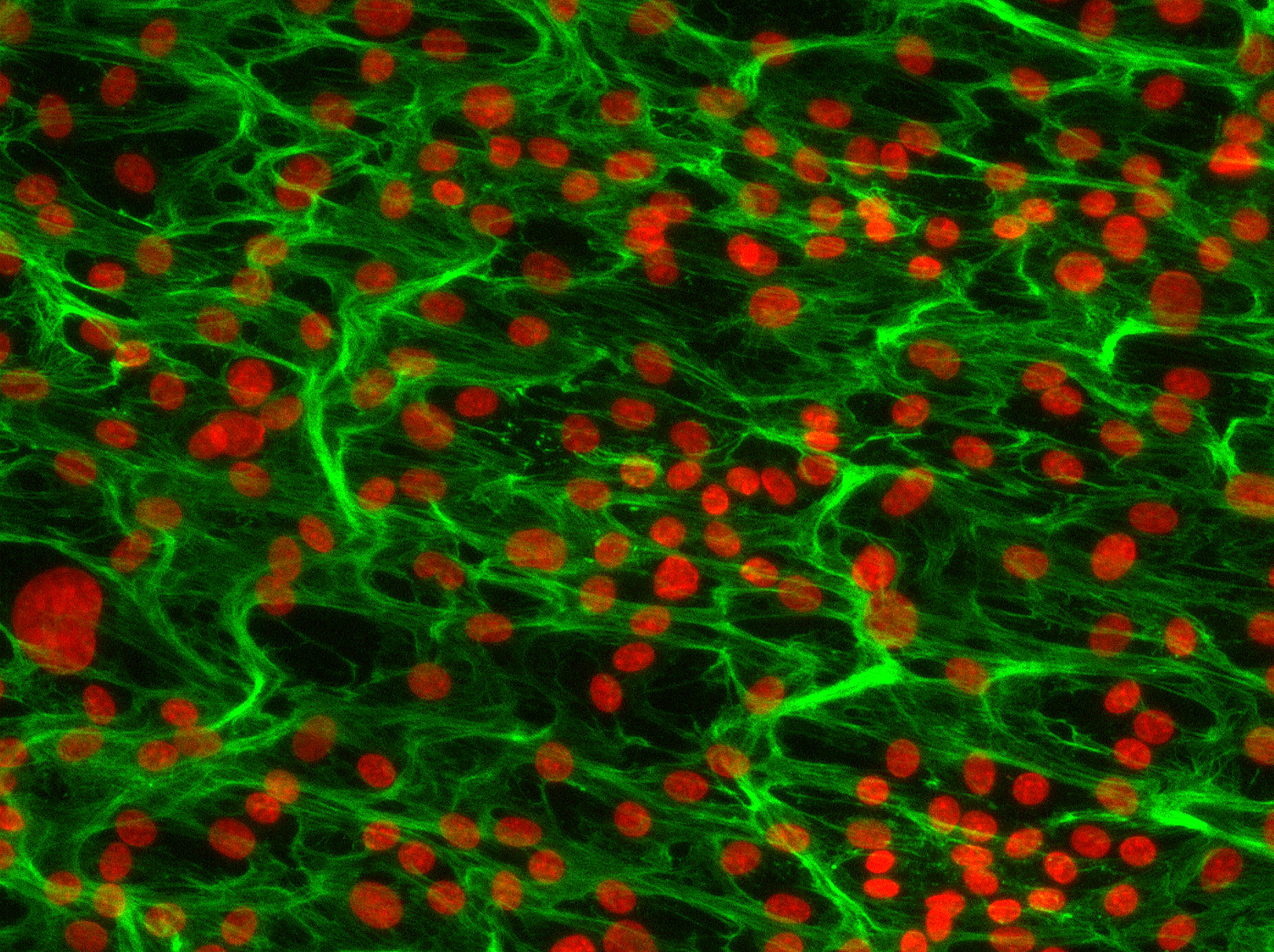
The blood-brain barrier is a highly selective filtering mechanism of capillaries that carry blood to the brain and spinal tissue. The barrier blocks certain substances to protect the brain from circulating pathogens in the blood. Endothelia line blood vessels and control the flow of substances between blood and tissue.
Increased leak of blood proteins across the blood-brain barrier occurs early in the progression of Alzheimer’s and related diseases, suggesting these changes may strongly contribute to disease progression. Additionally, these changes are often tied to impaired neuro-vascular coupling, the mechanism which allows blood vessels to increase flow in response to the energy needs of the working neurons.
Patrick Murphy, Center for Vascular Biology, in collaboration with Dr. Riqiang Yan of the Department of Neuroscience, have received a $2.2 million grant from the National Institutes for Health to investigate the changes in RNA regulation within the endothelial cells of the blood-brain barrier in the onset of neurodegenerative diseases like Alzheimer’s disease and Dementia.
Murphy’s group will look at splicing dysregulation within the endothelium caused by defects in the RNA-binding splice factor TDP-43, which is considered a hallmark of and potential contributor to cognitive decline in Alzheimer’s disease and Related Dementia.
The researchers identified low levels of TDP-43 in the endothelium of frozen banked human brain tissues from Alzheimer’s disease and Dementia patients using a novel method to isolate endothelia nuclei.
In animal models with endothelial-specific deletion of TDP-43, they have shown TDP-43 plays a role in the regulation of the blood-brain barrier endothelium. When TDP-43 malfunctions, the barrier is less effective at filtering out malignant particles from entering the central nervous system. These findings suggest there may be an important connection between the loss of this protein’s function in the brain endothelium and these diseases.
“Startup funds from the UConn School of Medicine and from an NIH K99/R00 transition award were critical for this novel high-risk high-reward work,” Murphy says, “which allowed me the time and resources to explore this with my research associate Amy Kimble, and summer and rotation students Jordan Silva and Nathan Leclair.”
In their basic studies to understand the effects of splice factor function within the endothelium, Murphy’s lab was surprised to discover a potent effect of TDP-43 dysfunction on endothelial activation, a critical component of nearly every inflammatory process in the body.
Murphy has been working with other investigators in the ImmunoCardiovascular Group and others in the Center for Vascular Biology. Murphy reached out to Yan for his expertise on Alzheimer’s disease for this project.
“His enthusiasm was contagious, and he said that there was a lot of interest in understanding how changes in the vasculature, and the blood-brain barrier in particular, might contribute to the progression of Alzheimer’s and other dementias,” Murphy says.
While the underlying mechanism is not yet clear, TDP-43 is best known as a splice factor. Splicing is the process by which non-coding segments of genes are cut out of the sequence as it is being transcribed to messenger RNA to become a protein. Proteins such as TDP-43 guide this splicing process to ensure proper translation and protein production.
Murphy hypothesizes that the loss of nuclear TDP-43 in the endothelium contributes to defects in the blood-brain barrier and microvasculature and thus leads to neurodegenerative diseases by affecting the splicing of pre-mRNA required for the maintenance of endothelium.
The researchers will examine TDP-43 expression and splicing activity in a range of neurodegenerative diseases linked to TDP-43 dysfunction and test the effect of the loss of nuclear TDP-43 on neurodegenerative disease progression in mouse models.
The team’s novel techniques provide them with an unprecedented molecular view of the endothelium in these disease states. They plan to extend their work on TDP-43 to broadly examine splicing alterations to determine whether defects in other endothelial splice factors also contribute to brain-blood barrier dysfunction.
Attaining a better understanding of the role of splice factors like TDP-43 within the endothelium in the onset and progression of Alzheimer’s and Dementia could provide a readily accessible target to slow disease progression, as drugs to target this process would not need to cross the blood brain barrier like those targeting neurons and other cells within the brain itself.
“With Dr. Yan’s help and the support of my department chair, Linda Shapiro, we developed a world-class team of collaborators in a field that is still new to me and embarked on this journey,” Murphy says. “I am grateful for the support of the NIH and very excited to continue this work in the next few years. We hope our novel focus on splicing regulation within the endothelium will provide new approaches to these devastating diseases.”
Murphy holds a Ph.D. in biomedical sciences from the University of California, San Francisco. He completed his postdoctoral training at the Massachusetts Institute of Technology in Richard Hynes’ Lab. Murphy’s research focuses on the interplay between recruited immune cells and the endothelial lining of the vasculature in chronic inflammation, specifically looking at alternative splicing and changes in the sub-endothelial matrix.