In 2019, Zambia had only seven radiologists—and no training program—for a population of 19 million.
In 2021, UConn School of Medicine radiologist Dr. Jill Wruble helped develop the didactic curriculum for the country’s first radiology residency, launching GlobalRadZambia (GRadZ), an international collaborative that brings radiologists together to teach, mentor, and build community. Since then, GRadZ has supported the residency through virtual instruction, periodic on-site teaching, and efforts to strengthen diagnostic capacity, including helping programs acquire essential equipment.
By 2023, the impact was clear. Twelve new radiologists had graduated—more than doubling the national workforce—and Zambia had begun training physicians from three neighboring countries without radiology programs.
“Watching these physicians discover the potential of radiology to improve patient care—and reshape the region’s future through hard-earned skill and determination—has enriched my life,” Wruble says.
Here, she describes her experience with the program, and the remarkable success it’s enjoyed.
Veronica, GlobalRadZambia, and the Making of Zambia’s First Radiology Residency

Regal in bright chitenge, Dr. Veronica Sunkuta Sichizya moves purposefully along the narrow paths winding through crowded, open-air courtyards at University Teaching Hospital in Lusaka. I walk beside her. We pass families crouching on the ground, mothers with children swathed to their backs, keeping vigil outside the wards day and night. Veronica has served these people for decades. The weight of that responsibility has only strengthened her resolve.

Veronica grew up one of fifteen children, raised by a father who insisted that all his children be educated. She completed her medical degree at the University of Zambia School of Medicine and later pursued advanced radiology training in South Africa, along with her neurosurgeon husband. She then returned to Zambia because her family was there and because serving her community mattered to her.

For decades, she had been the country’s radiologist-general, reading studies of chronic HIV and TB, complex trauma, and advanced cancers. She coaxed dilapidated machines back to life, working during the days and late into the nights. Her stamina and purpose, grounded in faith, never wavered.
Zambia’s First Radiology Residency
In 2019, despite an unrelenting workload, unreliable equipment, and inconsistent support, Veronica launched Zambia’s first radiology residency. It began with a few trainees (called “registrars”), no colleagues or subspecialists, no curriculum, little structure, and no teaching files. In its earliest months, the program partnered with Dr. Michael Potchen, neuroradiology professor at the University of Rochester, who helped begin building the curriculum and teaching files. Many doubted the program would survive. But the talent and drive of the registrars carried it forward.
Later, GlobalRadZambia (GRadZ) joined the effort—an international teaching collaborative that connects volunteer radiologists from the U.S. and abroad with Zambia’s trainees to provide structured didactics, case-based teaching, and mentorship. GRadZ became the program’s external academic partner, helping strengthen the residency’s educational foundation and expand the support available to Veronica and her team.
Our partnership began with a 2021 email—polite but urgent—from Dr. Mutale Chanda, then a junior registrar. She was convinced that the residency needed consistent didactics and a formal curriculum. Having audited the program I created for Tanzania’s residency at Kilimanjaro Christian Medical Centre, she knew Zambia needed a similar structure.
I asked the only question that mattered: Would her team be fully engaged? Mutale answered immediately and unequivocally: “Yes.”
I meant the requirement literally. Each resident would sign a multi-part pledge: to arrive on time, introduce themselves, keep their Zoom cameras on, participate in discussions, and, afterward, have one resident send a thank-you note on behalf of the group. Simple, but indispensable.
And GlobalRadZambia began.
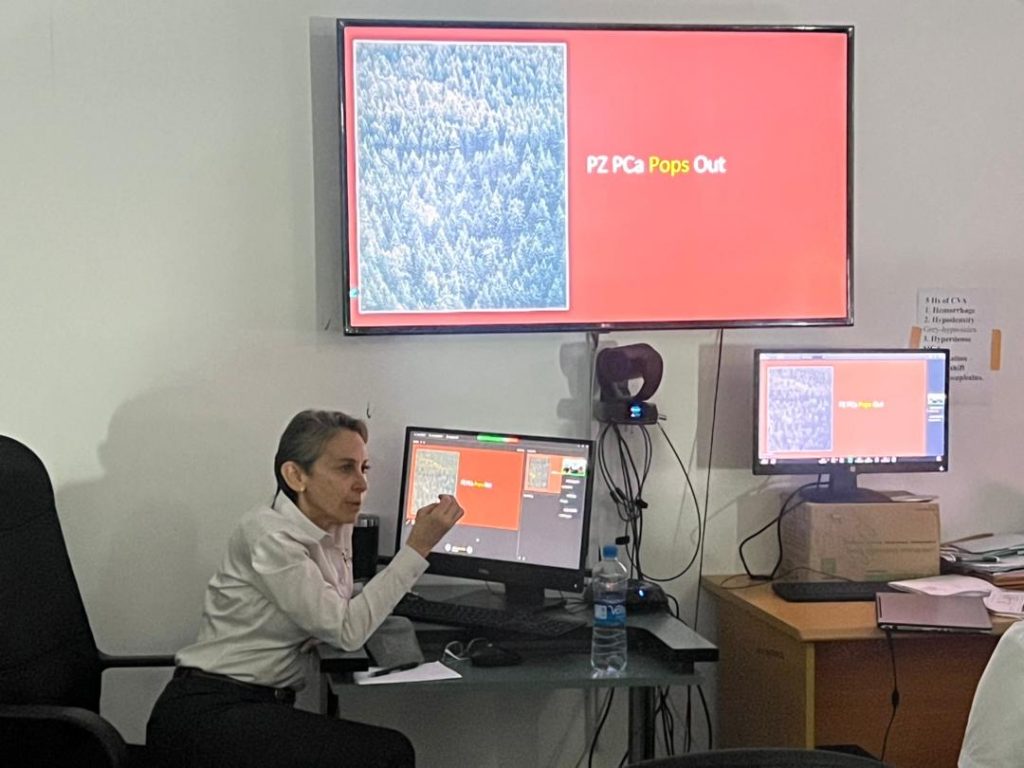
At first, it was a handful of faculty, a Zoom link, and registrars joining from clinics (or parked cars when the signal there was stronger). They arrived early—cameras on, prepared, curious. Their commitment drew faculty back. The teaching calendar stayed full.

Sessions became interactive, energized by shared purpose. The audience grew, confidence deepened, language shifted from tentative to precise, and radiologic eyes sharpened.
We felt the shift and a rare opportunity unfolding before us. We were helping train physicians who would not simply enter the radiology community but build one. They would shape how radiology is practiced across Zambia, establish credentialing standards, build screening pathways, improve outcomes, and become the nation’s first subspecialists.
Word spread. Faculty invited colleagues. Soon, more than forty radiologists volunteered—including breast, chest, body, neuro, musculoskeletal, nuclear medicine, pediatrics—from UConn, Johns Hopkins, Memorial Sloan Kettering, Yale, Loyola, private practices, Virtual Radiologic Associates, and colleagues in Sydney and Manila.
A Tipping Point

Even as support grew, the realities at University Teaching Hospital in Lusaka remained daunting. The 1,600-bed hospital debated adding bunk beds for capacity. Patients spilled into corridors, families slept beside beds, and some had traveled for days. Many arrived exhausted and gravely ill. Power outages were routine. The internet faltered. Bins of CDs sat unread because the systems were slow.
By 2023, twelve radiologists had completed training, nearly doubling the national workforce. Trainees came from Malawi, Congo, and Namibia because Zambia was becoming the place to learn. Graduates revitalized hospitals across Lusaka. One led breast imaging after training at MD Anderson. Another began a neuro-oncology fellowship at Memorial Sloan Kettering. A third won an international AI prize for a homegrown PACS designed with University of Zambia engineers.

A critical mass formed. Radiology was changing patient care.
We now needed a next step worthy of the program’s momentum and the registrars’ ambition. It was time to move beyond Zoom and design a purposeful on-site collaboration.
A family friend, Dr. Ashley Harris, a Harvard-trained internist committed to underserved care, joined us, moderating weekly Zoom meetings with UTH faculty who designed the next phase themselves: a staged POCUS curriculum and three incremental on-site visits.
Designing the Next Step Together
Support arrived with remarkable generosity. The Nielsen Foundation funded travel and essential logistics. The philanthropic arm of Virtual Radiologic—the world’s largest teleradiology practice—covered portable ultrasound devices (Butterfly units).

Butterfly’s own Global Health Program discounted their equipment and educational support. Radiology learning resources followed: CaseStacks donated full access to its case-review platform; the American College of Radiology contributed electronic texts, a full body-imaging course, and a scholarship to its four-week review program; and Medality/MRI Online provided educational access. To receive this charitable support, we created GlobalMedEd, Inc., and launched a website to acknowledge donors and share updates on globalmeded.org.
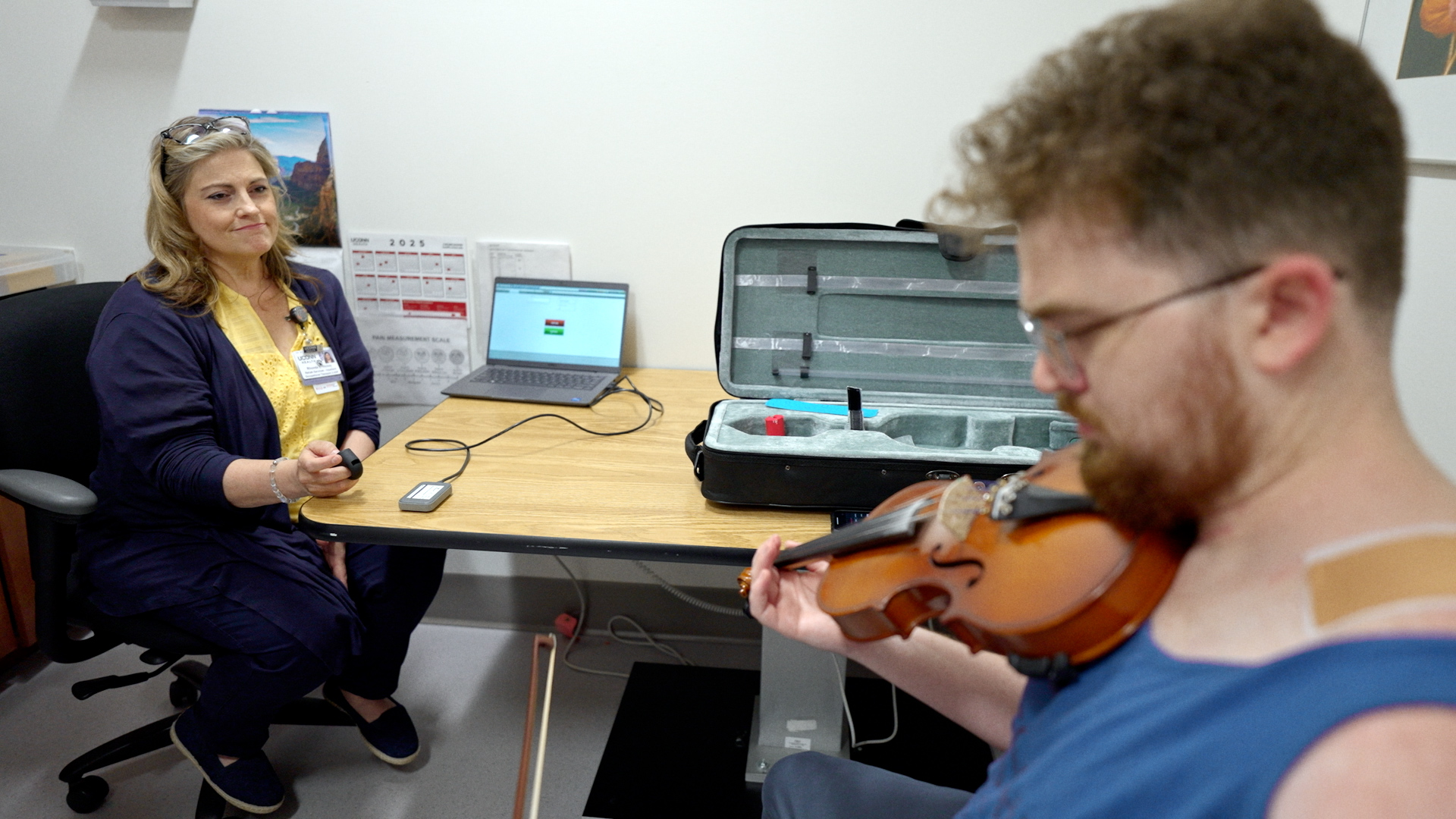
I formed an advance team and recruited the multi-talented Dr. Jon Vaccaro, who helped establish Guyana’s first radiology residency. Three exceptional technologists came on board: Susan Henson, UConn Health’s head ultrasound technologist; Danielle Brown, a gifted educator and curriculum developer; and Michelle Cunningham, who teaches ultrasound in Liberia and other resource-limited settings. All volunteered their time and worked together seamlessly, collaborating with the ease and trust of lifelong friends.
Dr. Harris guided the collaboration with UTH faculty. Curriculum outlines, protocols, workflows, and plans for an on-site program took shape piece by piece through shared documents, weekly calls, and meticulous planning.


Return to Zambia

Three and a half years had passed, and the groundwork was ready. It was time to meet the registrars in person and offer the intensive, structured teaching.
Three recent graduates and Veronica greeted me at the airport with bouquets and wide smiles. At her invitation, I stayed in her home. Our mornings began with grace, then the slow parade of cars on rutted roads.
Our days were full—with teaching, planning, and building partnerships. We coordinated with Christian Health Service Corps for a Mukinge Mission Hospital trip. I met with Zambia’s Minister of Health about digitizing backlogs. A University of Zambia engineer and resident, Peter Chibuta, presented their award-winning imaging system. Representatives from ACR and MEDALITY met virtually with residents and left deeply invested in their success.
Momentum accelerated. The registrars have begun to travel to hospitals in the Copperbelt and Northwest Province, which are still without radiologists. Requests are multiplying from across Zambia and as far away as Sierra Leone.

The Falls
Before leaving Zambia, I visited Victoria Falls—Mosi-oa-Tunya, “The Smoke That Thunders”—and watched the Zambezi River gather speed before cascading over the cliffs.
It made me think of UTH, where Veronica helped the registrars gather momentum of their own.

Momentum continued to build. The registrars have begun teaching in outlying provinces—including the Copperbelt and the Northwest—as requests multiply across Zambia, they are emerging as regional leaders.
At the same time, GlobalRadZambia prepares for its second and third ultrasound training trips to Lusaka and is also developing new partnerships to strengthen radiology education in a rural medicine residency in the Mississippi Delta and to support the launch of Sierra Leone’s first radiology residency.
I returned to UConn deeply grateful for the GlobalRadZambia team and for the faculty who have invested so fully in these registrars.