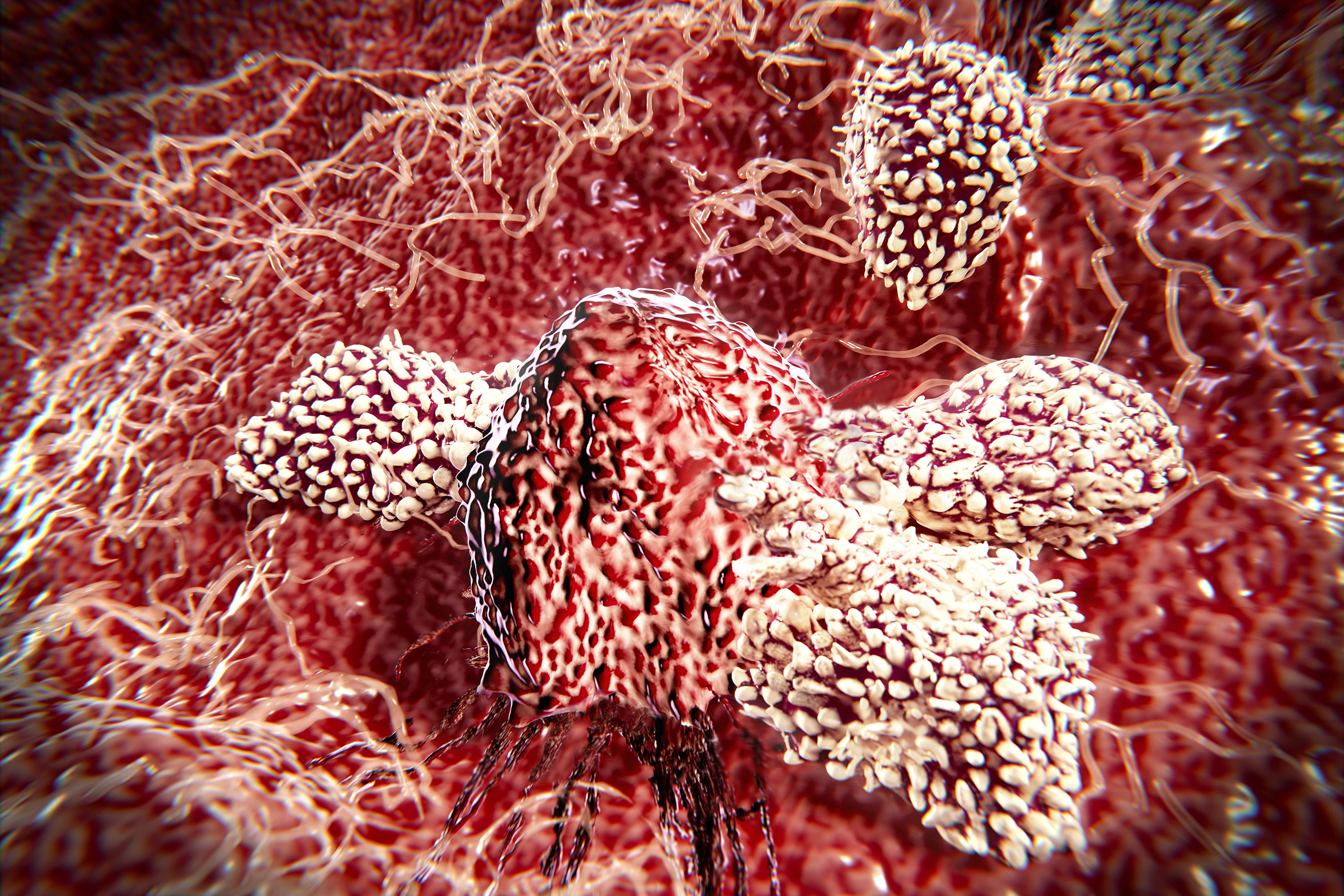
Immunotherapies are promising in theory, but often not in practice. In fact according to experts, they actually only work 10 percent of the time in the treatment of cancer – at best. Yet, while immunotherapy drugs may only help a minority of patients, those who do respond often do extremely well. As a result, many scientists are working to tap into the treatment’s benefits for a wider group of patients.
A team of researchers from UConn Health is among this group of scientists. They are developing a diagnostic and monitoring tool that can evaluate whether a patient suffering from cancer will respond to immunotherapy, before treatment even starts.
While immunotherapy holds incredible promise, it’s currently like going into battle with high tech weapons wearing a blindfold. — Veneta Qendro
In a recent issue of Proteomics, lead author Veneta Qendro, a graduate student in vascular biology, David Han, associate professor of cell biology, and team describe their platform technology, known as a Genomics Driven Immunoproteomics or GDI, which allows rapid identification of personalized tumor mutation profiles that are recognized by cancer patients’ own immune system. This new immune assessment tool has the potential to offer more effective treatment options for some of the most aggressive cancer cases.
“While immunotherapy holds incredible promise, it’s currently like going into battle with high tech weapons wearing a blindfold,” explains Qendro. “In patients who respond well, the outcomes are really significant, but without the personalized information about a specific patient and their unique mutations that invoke immune response, we’re just crossing our fingers and hoping it works. Using GDI helps make a more informed decision about what will be successful, and provides a map to adjust care for better results.”

To remove the immunotherapy blindfold, the technology identifies molecular and genetic insights about the unique immune response of an individual patient. Using a process called deep sequencing of high-frequency cancer genes by which the same region is analyzed multiple times, the UConn Health team identified variants found in 15 cancer patients that then served as a template to design a patient-specific peptide diagnostic tool. When incubated with blood from a cancer patient, the tool – also known as a microarray chip – indicates whether that patient’s immune system is producing any antibodies to attack against the mutation. It also shows which antibodies respond to which tumor mutations.
If there is no response, which is the case for the majority of patients receiving immunotherapies, clinicians can consider changing course and suggest alternative treatment options. If there is a response, both physicians and patients enter into a treatment plan knowing they are using the right weapon to battle the disease. Knowing whether patients will respond to treatment before it begins not only increases the likelihood of eradicating the disease, it also saves precious time, limits the occurrence of adverse side effects, and reduces costs for unnecessary and often painful therapies and procedures.
Patients screened using GDI whose immune systems do not produce antibodies against their disease could also benefit from the technology.
“Imagine two patients have the same mutation, but one is exhibiting an immune response with certain antibodies and the other has no response at all,” explains Han. “We can use the knowledge gained from the first patient to develop an immunotherapy that should theoretically have a higher chance of success in the second patient. It’s another example of how removing the blindfold could increase the impact of these treatments.”
While Qendro and Han are excited about the benefits their technology provides as a diagnostic and predictive tool, their big picture goal is to use the data collected from screenings to create a library of mutations and corresponding antibodies that work against them. With that information, they could develop personalized immunotherapy vaccines and antibody therapeutics to work with individual patients’ immune responses. Using these therapies in combination with other courses of care, such as checkpoint inhibitors, would help attack the disease from several fronts, the researchers say.
How to Reach Patients
Han and Qendro are exploring several options to advance the technology to the market where it can help patients and physicians. The pair recently formed a startup, Hans Health Inc., and have licensed the technology to pursue commercialization opportunities.
“Every day there is a wealth of technologies coming out of UConn and UConn Health labs that could improve the lives of citizens in our state,” says Radenka Maric, UConn’s vice president for research. “The University is committed to supporting faculty and student entrepreneurs through educational programming, patent and licensing expertise, seed funding, and industry mentorships to help early-stage ideas move beyond the lab, join the ranks of other successful Connecticut startups, and have an impact in our communities and our state economy.”
Qendro has taken the lead role in efforts to commercialize the technology as CEO of Hans Health Inc. She has participated in several entrepreneurship programs at UConn, such as the University’s NSF I-Corps site Accelerate UConn, the CCEI Summer Fellowship, and the Wolff New Venture Competition, to take on this complex mission while continuing her scientific research and doctoral studies. She and Han credit these programs with giving them valuable training to think like entrepreneurs as well as scientists.
For approximately 15 weeks, Qendro and the other would-be entrepreneurs in the Accelerate UConn and CCEI Summer Fellowship programs spent hours in the classroom and in the field, conducting interviews with potential customers. The goal was to understand the customer, channels, pricing, and other parts of the business model before actually launching a business.
“Most of my peers do not typically get this kind of training during their studies, knowing that our expertise is primarily focused on biological research,” says Qendro. “But entrepreneurship and innovation programs like Accelerate UConn are incredibly helpful tools for researchers who have the willingness, but lack the knowledge to transition these ideas to the marketplace. Participating not only familiarized me with a lot of new concepts from the business world, but also equipped me with the right skills to help further advance our technology so it can reach patients, provide valuable insights, and guide actionable options.”
Teams that successfully complete Accelerate UConn are much better positioned to succeed as entrepreneurs in the future, says UConn professor of business and CCEI faculty director, Timothy Folta. “One of the most potent criticisms of university technology commercialization is that technologists do not have a good understanding about whether customers really want their technology because they are enamored with it. Accelerate UConn aims to correct this bias.”
Although their day jobs keep them busy, Han and Qendro are excited about the future of Hans Health and the potential impact their innovation could have for patients suffering from cancer. This past summer, they submitted a provisional patent application and licensed the technology from UConn through their startup. They expect to complete the prototype of their diagnostic kit by March 2018, and will then begin seeking partnerships with molecular information or pharmaceutical companies interested in genomic profiling assays.
For more information and to apply to Accelerate UConn, visit accelerate.uconn.edu. The application deadline is Jan. 26, 2018.