Chronic and non-healing wounds—one of the most devastating complications of diabetes and the leading cause of limb amputation—affects millions of Americans each year. Due to the complex nature of these wounds, proper clinical treatment has been limited.
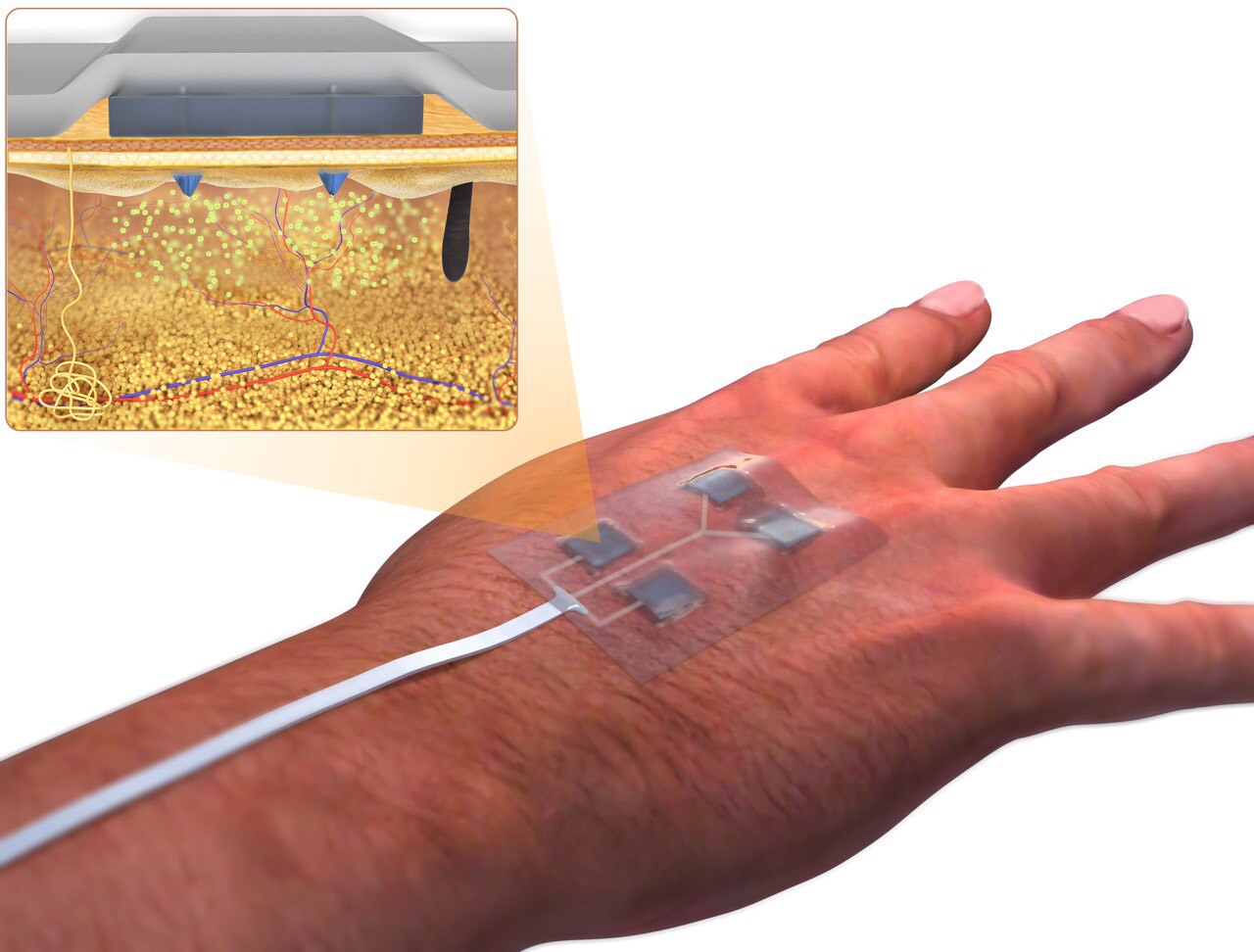
For the first time, faculty in the biomedical engineering department—a shared department with the UConn School of Dental Medicine, School of Medicine, and School of Engineering— designed a wirelessly-controlled, or “smart,” bandage and corresponding smartphone-sized platform that can precisely deliver different medications to the wound with independent dosing.
This bandage, developed by Dr. Ali Tamayol, associate professor, and researchers from the University of Nebraska-Lincoln and Harvard Medical School, is equipped with miniature needles that can be controlled wirelessly—allowing the drugs to be programmed by care providers without even visiting the patient.
“This is an important step in engineering advanced bandages that can facilitate the healing of hard to treat wounds. The bandage does not need to be changed continuously,” says Tamayol.
Given the range of processes necessary of wound healing, different medications are needed at different stages of tissue regeneration. The bandage—a wearable device—can deliver medicine with minimal invasiveness.
With the platform, the provider can wirelessly control the release of multiple drugs delivered through the miniature needles. These needles are able to penetrate into deeper layers of the wound bed with minimal pain and inflammation. This method proved to be more effective for wound closure and hair growth as compared to the topical administration of drugs, and is also minimally invasive.
The research, recently published in the Advanced Functional Materials journal, was first conducted on cells and later on diabetic mice with full thickness skin injury. With this technology, the mice showed signs of complete healing and lack of scar formation—showing the bandages’ ability to significantly improve the rate and quality of wound healing in diabetic animals.
These findings can potentially replace existing wound care systems and significantly reduce the morbidity of chronic wounds—which will change the way diabetic wounds are treated.
Tamayol recently applied for a patent for this technology.
This research was supported by the National Institutes of Health #R01GM126831