For rheumatologic conditions like rheumatoid arthritis and osteoarthritis, NSAIDS are often the first line of medications used for pain relief. UConn Pharmacy researchers have discovered a way to minimize the side effects associated with the treatment and bring it to market.
Nonsteroidal anti-inflammatory drugs (NSAIDS) are widely used to relieve pain, reduce fever, and bring down inflammation. More than 30 billion doses are taken each year — making them among the most popular medications worldwide for general pain relief.
But, there’s a downside. The most common dosage forms of NSAIDS are tablets and suspensions, which require patients to take the medication orally. When taken over a long period of time, NSAIDS can cause digestive problems like nausea and gastrointestinal bleeding. This causes a big problem for those who experience chronic pain and rely on NSAIDS to help.
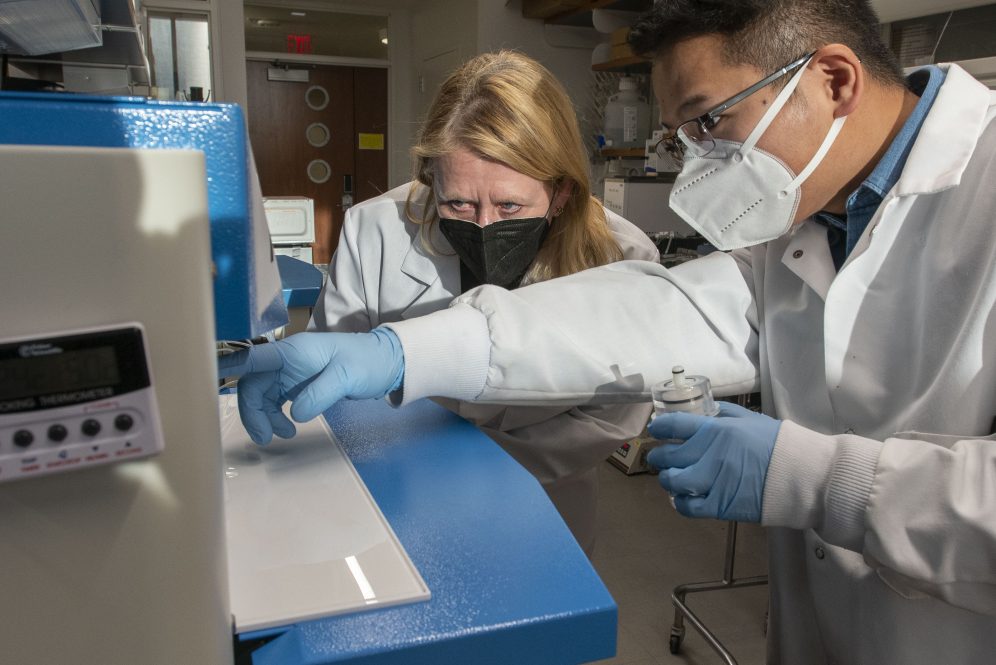
To address this issue, Board of Trustees Distinguished Professor of Pharmaceutics Diane Burgess and co-inventor and research assistant Professor Xiaoyi Wang developed a new technology with the potential to administer NSAIDS long-term and reduce or eliminate these side effects: long-acting injectable in situ forming biodegradable implants.
In situ forming implants are defined as liquid formulations that generate solid or semisolid depots following administration. This form of delivery allows for the sustained release of drug over periods of days to months while avoiding any side effects that might be associated with oral administration.
According to Burgess, who is also the Pfizer Distinguished Endowed Chair in Pharmaceutical Technology, the injection is made up of a polymer solution with solvent. The solvent diffuses away from the injection site once it’s in the subcutaneous space under the skin. This allows the polymer to solidify and slowly release the drug over time. And, since the polymer is made up of lactic acid and glycolic acid units which are naturally already found in the body, the implant is fully biodegradable and biocompatible.
“There’s no toxicity associated with it,” Burgess says. “It will degrade away by itself as the drug is released.” This means that no surgery is needed to either implant or remove this dosage form — making these in situ forming implants far less invasive than traditional solid implants.
When it comes to patient compliance, this particular dosage form comes in handy. Patients who are prescribed NSAIDS long-term might have to take two or three tablets, three times daily or more to control the pain, says Burgess, but one injection using this technology can last up to six months — releasing the drug in a controlled manner over time.
“When taking a drug for more than a week, patients tend to start forgetting to take it or just become less and less compliant,” she says. For patients who need to take NSAIDs long term, in situ forming implants can be a convenient option.
This technology has the potential to be very helpful for a great number of people, Wang says. “And that’s the most important purpose.”
With the help of UConn Technology Commercialization Services (TCS), Dr. Burgess’ and Wang’s technology was successfully licensed by ForDoz Pharma in December 2022.
“This technology is a platform technology and allows for sustained release of NSAIDs over a period of days to months, that allows for long-term use of NSAIDs, reduces side effects, and improves patient compliance,” says Amit Kumar, senior director of licensing for TCS. “We are happy to work with ForDoz Pharma on maturing this technology further and bringing it to the market.”
Based in New Jersey, ForDoz is a privately-owned specialty pharmaceutical company focused on the development, manufacturing, and commercialization of sterile complex injectable products.
“This technology fully matches our pipeline,” says James He, co-founder and CEO of ForDoz. “We want to be the pioneer in the pharmaceutical area of complex injectables, and there are not many products out there that utilize this technology.”
He, along with co-founder and Chief Scientific Officer Dr. Sydney Ugwu are currently working on fully developing a commercial product that can be manufactured on a large scale and put on the market.
“I’m hoping that we can commercialize the technology soon and that we can collaborate with UConn in other areas in the future,” says Dr. Ugwu.