One in every three adults in the US suffers from some type of chronic pain. While there are treatment options to mitigate most kinds of chronic pain, visceral pain has no effective treatment options.
While visceral pain poses a major clinical challenge, developing new treatments, especially non-drug alternatives requires more knowledge about the mechanisms behind it. With a new grant from the National Institutes of Health, two UConn researchers aim to increase knowledge about this widespread clinical problem, which could one day lead to improved treatment options for patients suffering from chronic visceral pain.
Bin Feng and Guoan Zheng, professors in the Department of Biomedical Engineering, have recently received a $2,030,740 grant from the NIH’s National Institute of Neurological Disorders and Stroke to better understand the causes of chronic visceral pain in patients with irritable bowel syndrome (IBS). IBS affects about 15% of the population in the US, and chronic visceral pain is one of the main symptoms of the disorder.
The UConn research team plans to use this funding to characterize the sensory neural cell bodies in a cluster of neurons known as the dorsal root ganglion, or DRG. These neural clusters are responsible for transmitting sensory messages of pain and touch from skin, as well as inner abdominal organs including the colon and rectum.
Feng and Zheng will quantify the topological distribution of pain receptors called mechanonociceptors. These neurons respond to intense pressure on the colorectum. These pain receptors are awakened by tissue inflammation and respond to a mechanical, thermal, or chemical stimulus. This project will help to define the molecular properties of mechano- and silent nociceptors, specifically in the thoracolumbar and lumbosacral DRG.
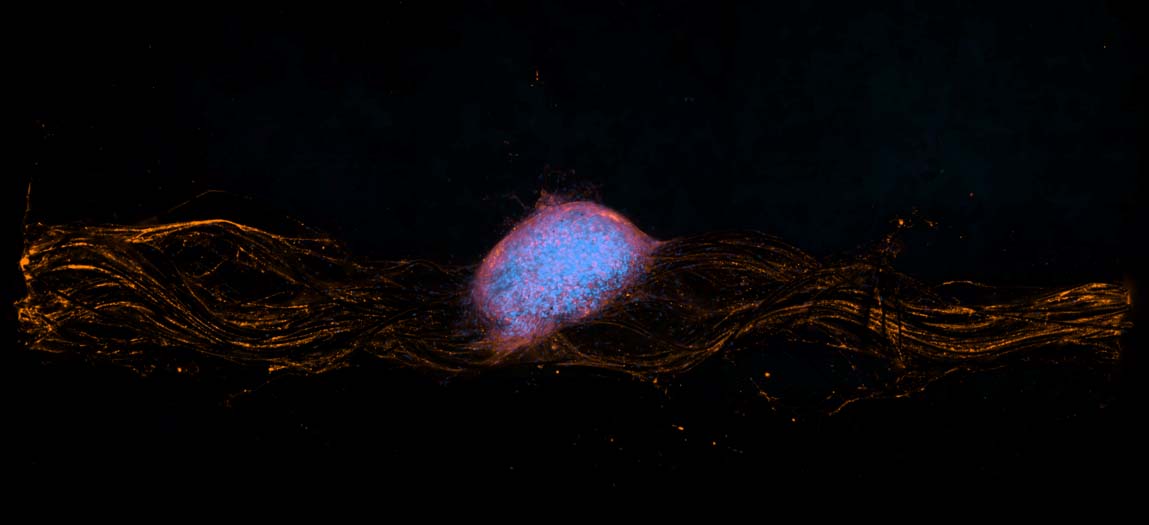
With this funded grant, the Feng and Zheng labs will determine the function and molecular profiles of those DRG neurons by using a cutting-edge optical recording setup that is currently under development. The setup detects faint fluorescent light signals from genetically modified calcium/calmodulin-dependent protein kinase (CAMK) in DRG neurons at a high sensitivity and recording rate. With this novel optical recording approach, the neural encoding functions of DRG neurons supplying nerves to the colon and rectum can be studied at a much higher efficiency compared to conventional approaches which rely on electrical recording.
“Outcomes of this study will fill our gap in knowledge, which is crucial and will help guide the development of non-drug alternatives, including neuromodulation to treat chronic visceral pain by selective targeting of the DRG,” says Feng.
Bin Feng is an assistant professor of biomedical engineering at the University of Connecticut. His research interests lie in neural engineering, neuromodulation, electrophysiology, experimental and computational neuroscience and soft tissue biomechanics with a focus on the sensory encoding and processing of the peripheral nervous system. He received his Ph.D. in biomedical engineering from Purdue University at West Lafayette and completed postdoctoral research in visceral pain and neuroscience from the University of Pittsburgh.
Guoan Zheng is the United Technologies associate professor in biomedical engineering at the University of Connecticut. Zheng is a leading expert in developing innovative biomedical imaging devices and algorithms. In particular, he led the development of the Fourier Ptychography approach that embodies a new way of tackling microscopy by transforming a physical optical problem to a computational problem. Zheng received his Ph.D. in electrical engineering from California Institute of Technology.
This project is award number: 1U01NS113873-01