Vijay A. K. Rathinam, an assistant professor in UConn Health’s Department of Immunology, recently received nearly $440,000 from the National Institutes of Health and the National Institute of Allergy and Infectious Diseases to study an ill-understood response to bacterial infection that can have dangerous and deadly consequences.
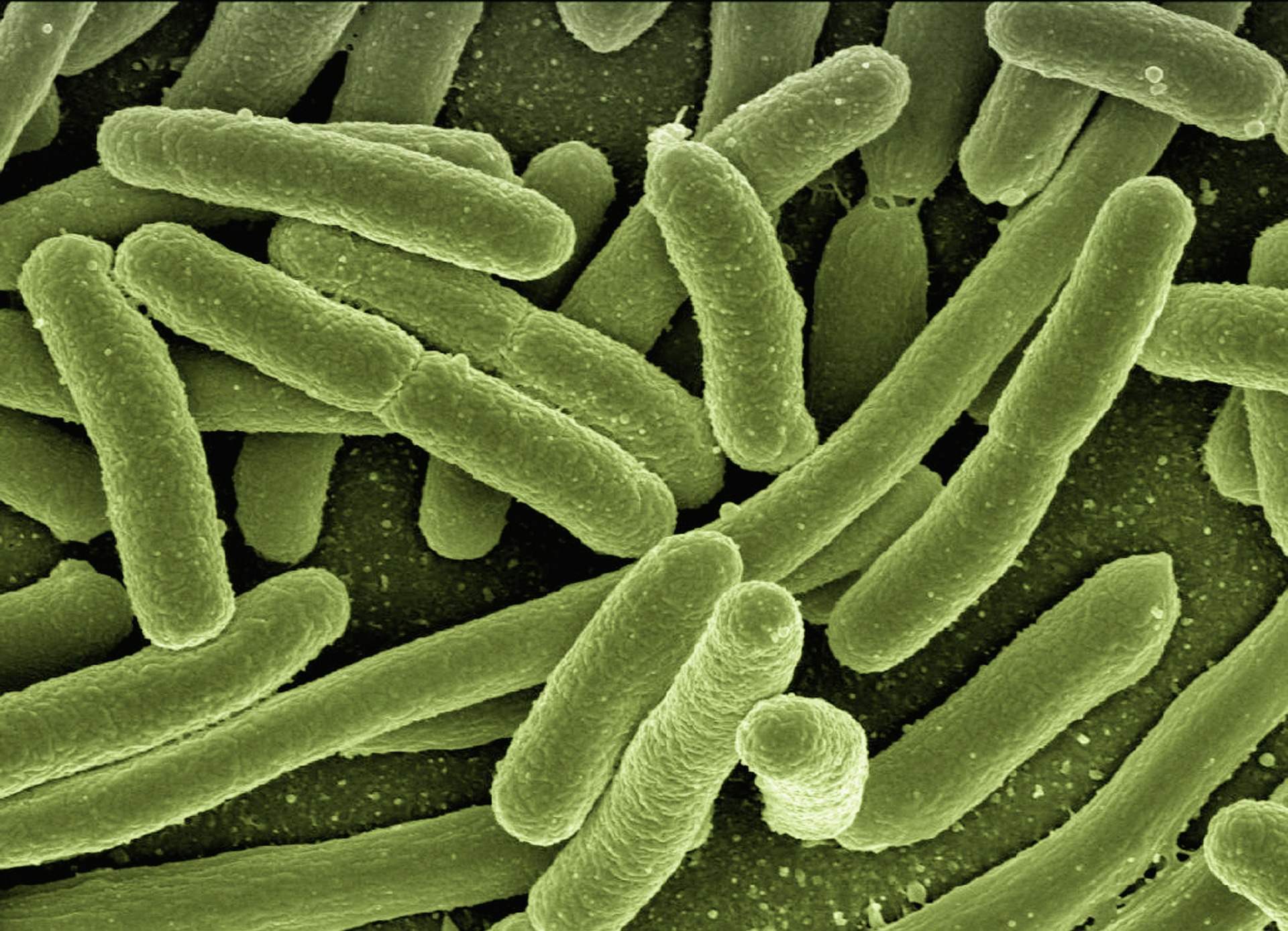
Sepsis is the body’s extreme reaction to bacterial infections. Sepsis causes severe damage to the lungs, kidney, and gut. If this condition is not treated quickly, it can be fatal.

assistant professor of immunology at UConn Health. (UConn Photo)
Inflammasomes are multiprotein structures that are responsible for the activation of our bodies’ inflammatory responses to foreign pathogens. Lipopolysaccharides (LPS) are large molecules found in the outer membrane of certain bacteria that maintain the integrity of bacterial membranes and protect them from certain kinds of chemical attacks. When inflammasomes sense the presence of LPS inside the cell, the immune system is triggered to attack the bacterial infection. While the engagement of this pathway helps protect the host during bacterial infections, its excessive and prolonged activation can cause sepsis.
Current knowledge of how this response contributes to host defense against bacterial infections as well as sepsis is lacking. One of the outcomes of the activation of the caspase-11 protein, which is implicated in the response, is the release of intracellular proteins. These proteins act as alarmins, or damage associated molecular patterns, which incite and manage inflammatory responses to fight bacterial invaders. The unconventional protein secretion that results from the activation of this protein by cytosolic LPS is poorly understood.
“The identification and characterization of proteins secreted following innate immune sensing of LPS in the cytosol has the potential to reveal new therapeutic targets in sepsis, which is a highly lethal manifestation during infections and has no specific treatments,” says Rathinam.
Ashley Russo, Rathinam’s graduate student, in collaboration with UConn Health professors, Anthony Vella and Antoine Menoret, identified a novel alarmin involved in the regulation of innate immune responses during bacterial infections and sepsis, which this NIH-funded project will explore. This research has the potential to identify new biomarkers and targets to intervene in sepsis before it severely harms the host.
Rathinam received his postdoctoral training at the University of Massachusetts Medical School. His research focuses on understanding the immunological basis of infectious and inflammatory diseases.
This project is number: 1 R21 AI135528-01A1.