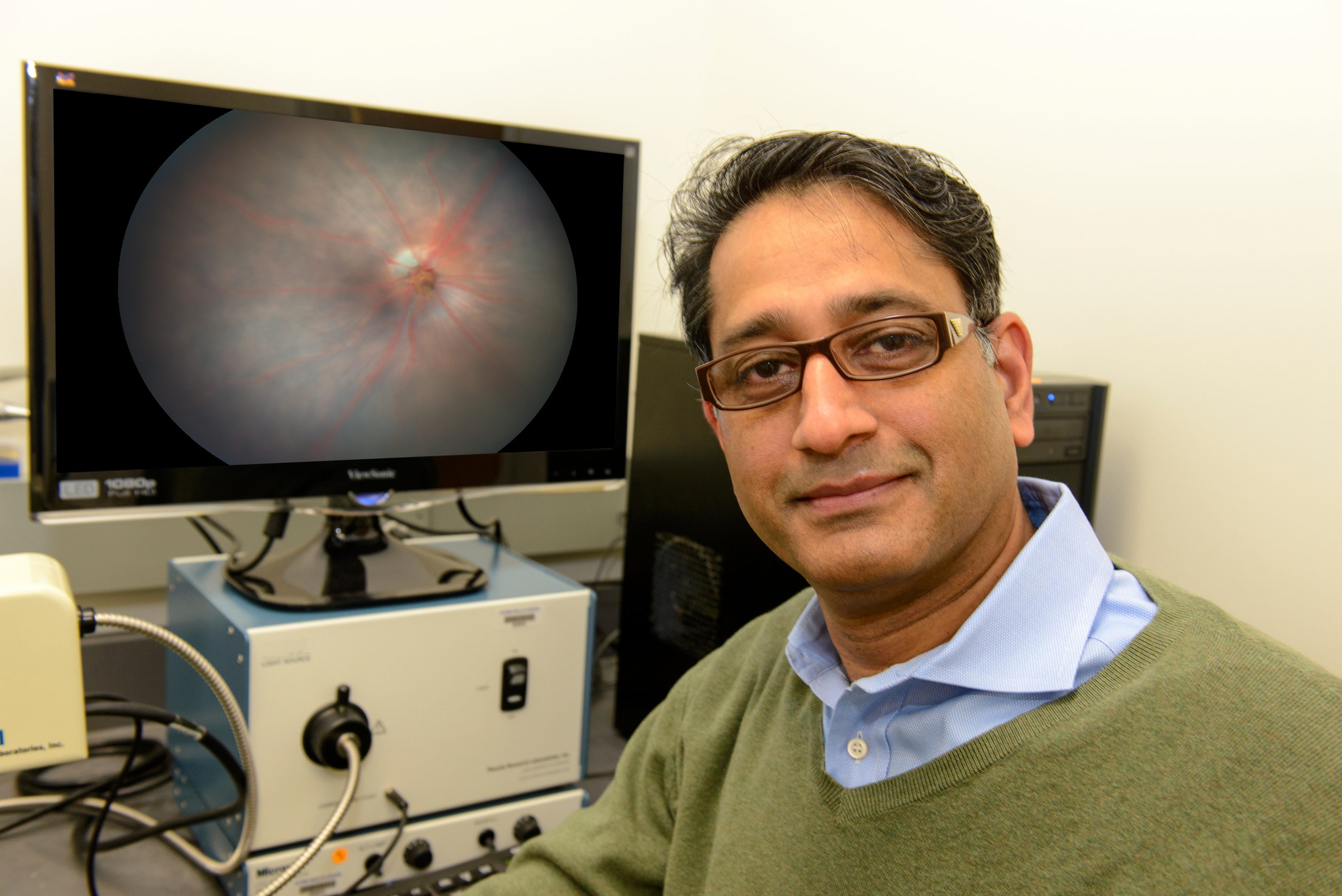
Royce Mohan, a UConn Health associate professor of neuroscience, has received more than $400,000 from the National Institutes of Health to study the role of a specific enzyme in retinal gliosis.
Age-related Macular Degeneration (AMD) is the most common cause of blindness in people over the age of 50 in many developed western countries, including 11 million Americans. Estimates predict that 196 million people worldwide will suffer from this condition by 2020. Retinal gliosis is a phenomenon that causes scarring and occurs in many eye diseases and also after injury.
With retinal gliosis, Muller glial cells become activated and can proliferate and become invasive. Gliosis has been observed in humans with AMD, as well as mouse models of AMD, signifying that a link exists between this process and the condition, but the details of the relationship remain unclear.
As AMD progresses people may begin to see a blurry spot at the center of their vision which will continue to develop into blank spots in one’s central vision. These effects are caused by damage to the macula, a one-mm sized tissue at the center of the retina that controls visual acuity. This loss of central vision interferes with every day tasks like reading, driving, and identifying faces. Elderly people lacking this central vision are also more prone to fall and break bones.
In the more severe form of AMD known as wet-AMD, the growth of new blood vessels from the retinal posterior choroidal layer can promote further damage by inducing scar formation. As tackling this enigma has not been successful in the clinic, Mohan and his former graduate student John Wizeman employed first a chemical model of retinal injury to study how gliosis contributes to scarring and examined intermediate filament proteins that become expressed in Muller glia. They showed that the filament protein GFAP (glial fibrillary acidic protein) undergoes the posttranslational modification called citrullination. Citrullinated proteins have been detected as disease-specific biomarkers in several major inflammatory diseases, such as rheumatoid arthritis and multiple sclerosis. Citrullination is an irreversible change in numerous critical protein targets that is caused by peptidyl arginine deiminase (PAD) enzymes. In this previous work, Mohan found that AMD patients with increased citrullinated proteins, which suggested the possibility that a certain PAD enzyme may be playing a key role in retinal gliosis.
Important insights into this retinal pathology came when Mohan found that activated Muller glia and retinal astrocytes, both of which are implicated in AMD, displayed elevated levels of GFAP that was citrullinated. Consequently, using a PAD inhibitor to target the citrullination process, they found this treatment restored GFAP to its near-native state. Deducing which PAD was responsible from a series of experiments led them to discover that PAD4 played the major pathological role in the chemical injury model.
Armed with this new knowledge, Mohan’s group proposed a high-risk/high-reward R21 grant to the National Institutes of Health to study PAD4 as a candidate for AMD. This grant will afford Mohan and his team to test if PAD4-driven citrullination controls chronic gliotic response in a laser-injury model of AMD that features choroidal neovascularization. The project will help determine if PAD4 is a potential target for pharmaceutical treatment in living organisms and will lay a foundation to probe this druggable target in conditions that cause irreversible blindness, like AMD.
“Interdisciplinary research can be very rewarding,” Mohan says, “especially when there are multiple challenges to overcome in a very short time and your ideas have to pan out.”
Mohan is cautiously optimistic and at the same time excited that this research could illuminate a new target for AMD.
“It is important to realize one can learn from other fields researching the links between citrullination and chronic diseases,” he says. “But we also have to pivot with bold new ideas through innovation and take risks.”
This project is number: 1R21EY028699-01.
Mohan received his Ph.D. from Ohio State University in biochemistry. He completed his postdoctoral work at the New England Medical Center, Tufts University School of Medicine and Brigham and Women’s Hospital, Harvard Medical School. The Mohan Lab focuses on researching new targets for ocular diseases that are undermined by pathological angiogenesis, fibrosis, and gliosis.