A patient noticed popping and clicking in their jaw after wisdom teeth removal. An IT professional working at a computer started to feel jaw and neck pain. A gum chewer suddenly felt pain in their cheeks when moving their jaw.
What do all of these situations have in common? They are common symptoms of temporomandibular joint disorders, or TMD—which affects up to 12% of adults in the United States.
In recognition of National Temporomandibular joint (TMJ) Awareness month, Dr. Seema Kurup, assistant professor and course director of Orofacial Pain and TMD at the UConn School of Dental Medicine answers the most frequently asked questions about TMD.
Q: What is TMD?
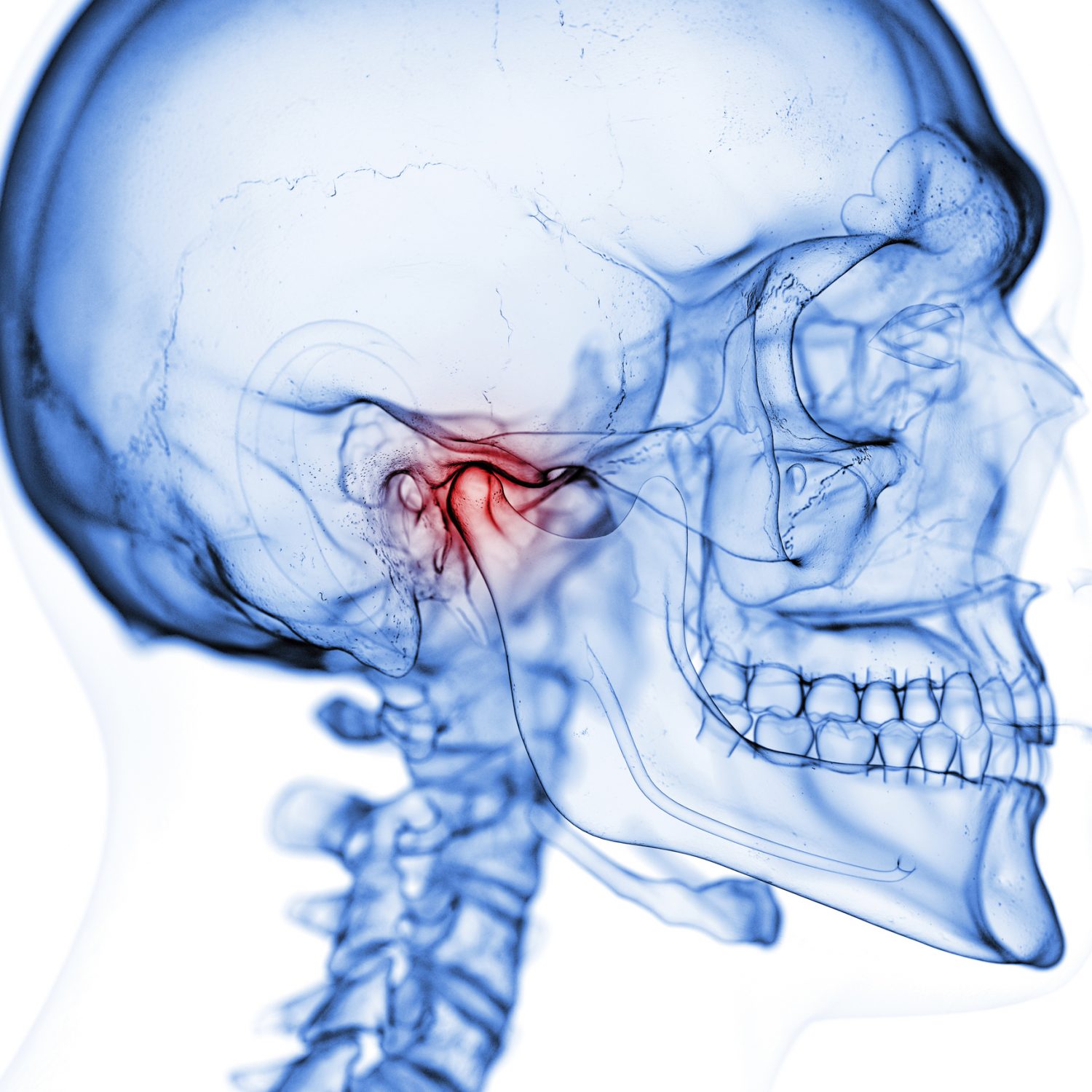
TMD or temporomandibular joint disorders are a group of conditions that cause pain and dysfunction in the jaw joint and muscles that control the jaw movement. The jaw joint or the temporomandibular joint (TMJ) connects the jaw to the skull and it lies in front of each ear. Many times, one may hear TMD wrongly called the ‘TMJ’.
Q: How do you recognize the signs and symptoms of TMD?
- Pain or tenderness in the jaw joint area, temple and in or around the ear when one chews, speaks, or open mouth wide
- Jaws that get “stuck” or “lock” in the open- or closed-mouth position
- Decreased mouth opening
- Clicking, popping, or grating sounds in the jaw joint when opening or closing the mouth which may or may not be painful
- Trouble chewing or a feeling of abnormal or uncomfortable bite — as if the upper and lower teeth are not fitting together properly
- Sometimes, headaches, earaches, upper shoulder & neck pain, ringing in the ears, and swelling
Q: What are the causes of TMD?
TMD may arise from a single cause or multiple associated causes. Few common causes are:
- Injury to the jaw, head or neck
- Grinding or clenching of teeth
- Dislocating the disc or soft tissue between the jaw joint and the skull bone
- Osteoarthritis or rheumatoid arthritis in the TM joints
- Conditions strongly associated with TMD: stress/depression, chronic low back pain, headache, sleep apnea.
Q: At what age does TMD manifest?
It is safe to say that many symptoms of TMD arise in adolescence or the early twenties and thereafter may continue intermittently, well into middle age. It is also more commonly seen in women.
Q: What are the treatments for TMD?
The current evidence-based and standard recommendations are to use conservative and reversible treatment as much as possible. Permanent and/or invasive procedures are considered only when necessary. Most patients do not need such aggressive treatment and simple self-care practices help ease most TMJ problems. In many patients, less is more and the best.
Q: How is TMD linked to overall orofacial pain?
Orofacial pain arises from various debilitating conditions involving the head, face, and neck. Since, TMD involves the masticatory muscles, the temporomandibular joint or both, causing multiple clinical problems, it is considered a highly prevalent orofacial pain condition for which patient seeks treatment.
To learn more about temporomandibular disorders, please visit the website for health information from the National Institutes of Health: https://www.nidcr.nih.gov/health-info/tmj/more-info
References:
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28(1):6–27. doi:10.11607/jop.1151
Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management, Sixth Edition. de Leeuw, Reny; Klasser, Gary (editors)
Meloto CB, Slade GD, Lichtenwalter RN, Bair E, Rathnayaka N, Diatchenko L, Greenspan JD, Maixner W, Fillingim RB, Ohrbach R. Clinical predictors of persistent temporomandibular disorder in people with first-onset temporomandibular disorder: A prospective case-control study. J Am Dent Assoc. 2019 Jul;150(7):572-581.
http://www.iadr.org/INfORM/DC-TMD
https://www.ncbi.nlm.nih.gov/pubmed/23809304
https://www.nidcr.nih.gov/health-info/tmj/more-info
https://my.clevelandclinic.org/health/diseases/15066-temporomandibular-disorders-tmd-overview