UConn Health today announced a revolutionary precision technology now available that is making early diagnosis of lung cancer easier than ever.
Lung cancer is the deadliest cancer for both men and women in the U.S. by a wide margin. More people die of lung cancer each year than of colon, breast, and prostate cancers combined, and more than half of people with lung cancer die within a year of being diagnosed, according to the American Lung Association. When the cancer is detected early, before it has had a chance to spread beyond the lungs, the five-year survival rate jumps from 5 to 56 percent.
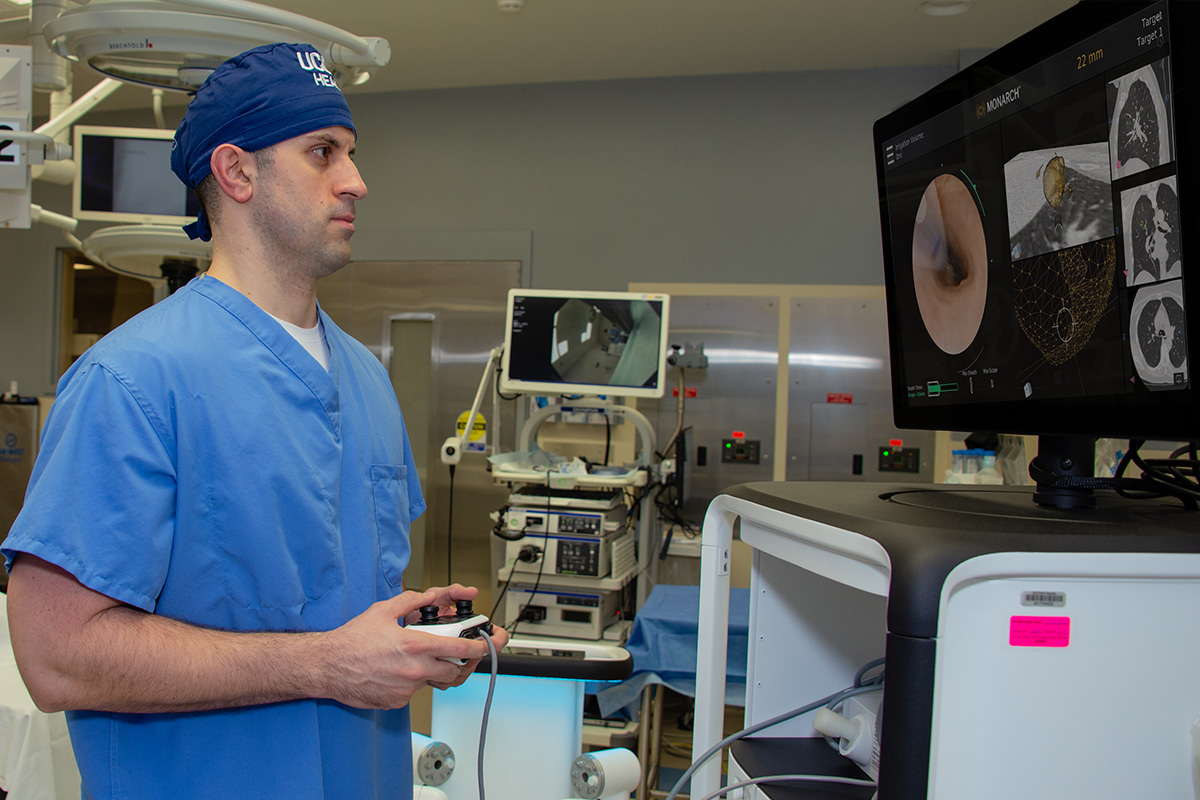
UConn Health is the first hospital in New England and among the first in the nation to offer robotic bronchoscopy on the Monarch platform from Auris Health, allowing physicians to quickly diagnose lesions detected through low-dose CT scans, including those that are small or in hard-to-reach parts of the lung.
“Before this technology, the targets would’ve had to be bigger. I wouldn’t be able to make certain angles without the robotic arm to navigate,” says Dr. Omar Ibrahim, UConn Health director of thoracic oncology and interventional pulmonology. “I have a higher degree of confidence and accuracy with this than with prior equipment.
“The ability to diagnose the cancers at an earlier stage will allow us to work towards surgical management of the disease,” he says.
With its instinctual, video-game-style controller, the Monarch platform allows the physician to move the endoscope up and down, left and right, forward and backward through the lung and its bronchi. Buttons on the controller make the scope of view bigger or smaller, while others control suction or irrigation.
Procedures are done in the operating room under general anesthesia. Within about an hour, the doctor will biopsy the suspicious nodule and a lymph node for analysis by a pathologist. The patient can go home the same day.
If cancer is confirmed in the lung, it will then be staged to see how far it has advanced. A team of cancer specialists then develop an individualized treatment plan that is ideal for the patient and their specific type and stage of cancer. A patient’s treatment plan might include surgery to remove a small portion of the lung or the entire lung, radiation therapy, chemotherapy, medications, and immunotherapy.
Not only does earlier diagnosis improve patients’ chances for survival, but it also helps reduce unnecessary stress, says Wendy Thibodeau, the lung cancer nurse navigator at UConn Health’s Carole and Ray Neag Comprehensive Cancer Center.
“We have had patients where initial and subsequent biopsies are inconclusive. A decision then has to be made: remove the nodule surgically, or watch it for growth,” Thibodeau says.
“This can be stressful on a patient. They either have to go through a significant procedure they may not have needed or wait to see if the nodule gets worse. This technology will give us better accuracy for appropriate tissue sampling, making the decision more clear.”
Routine screenings of high-risk patients — those with histories of smoking, especially — using low-dose CT scans and minimally invasive techniques help detect and diagnose more people all the time. The Monarch platform is the next step in improving outcomes for lung cancer patients, and Ibrahim sees even more groundbreaking advances on the horizon.
In his time at UConn Health, Ibrahim has worked to improve the experience of UConn Health’s lung cancer patients, particularly through a consolidated team that allows patients to come to one clinic to see a variety of doctors.
“Since we’ve enhanced and personalized the way we care for lung cancer, the number of lung cancer patients at UConn Health has quickly increased,” says Ibrahim. “Time to diagnosis and start treatment is tremendously shorter, and patients are happier with the quality of their care.”
He believes the robotic bronchoscopy technology will allow the team to deliver even better results.
“The accuracy of this is going to pan out to be second to nothing,” says Ibrahim. “I think this is the tip of the iceberg in diagnosis, and the therapeutic aspect of it, which will evolve over time, is really exciting. Being at the forefront of that is amazing.”
To refer a patient to the thoracic oncology team, call the dedicated line for referring physicians: 860-679-5555.
To request an appointment, call 860-692-8455.