In a cat-and-mouse game, sometimes the cat wins and sometimes it’s the mouse.
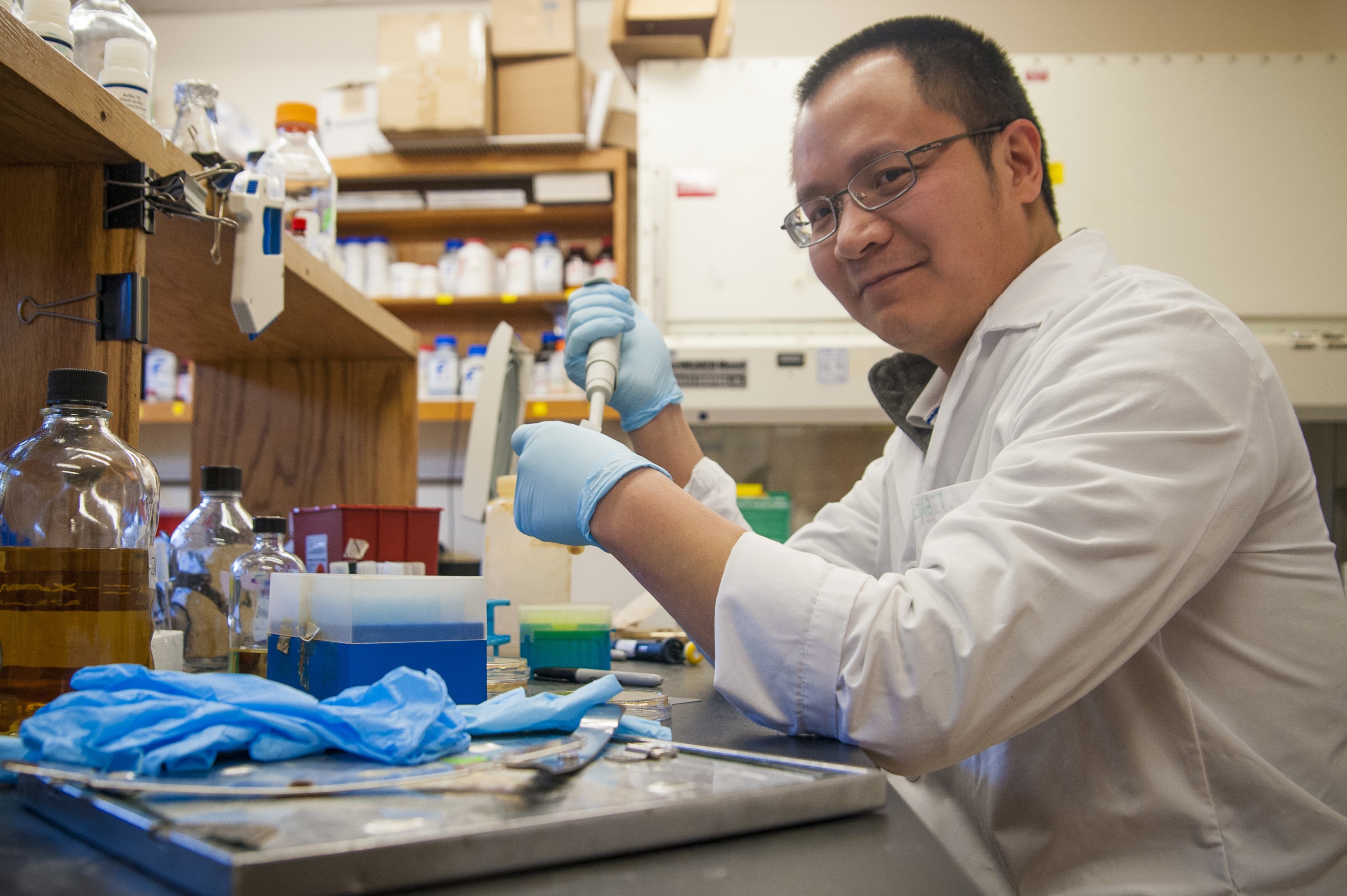
In groundbreaking research that is featured in the Feb. 1 early edition of the Proceedings of the National Academy of Science (PNAS), pathobiologist Xiaohui Zhou and his colleagues present their discovery of a protein called histidine kinase on the surface of certain vibrio bacteria – think the ‘bug’ that may cause diarrhea when we eat undercooked seafood.
This sentinel protein … only becomes active when it detects a beta-lactams antibiotic. It’s almost as if the antibiotic sets off an alarm bell and the protein leaps into action. — Xiaohui Zhou
This protein acts as a sentinel and when it detects the presence of antibiotics in the beta-lactams family – widely-used drugs that include penicillins and cephalosporins that are traditionally effective in fighting bacterial disease – it alerts the bacteria to produce an antibiotic-fighting enzyme called beta-lactamase.
And that’s when the eternal battle between disease-causing bacteria and the antibiotics designed to kill them begins in earnest. It’s like a cat-and-mouse game, where the bacteria takes the role of the mouse as it develops ways to outsmart the crafty opponent that’s intent on hunting it down.
The beta-lactamase enzyme works to degrade – or effectively disable – the antibiotic, and prevents it from penetrating the bacteria’s cell wall.
And that’s not all.
“One of the most intriguing findings coming out of our research is that histidine kinase – this sentinel protein – is not awake all the time. It only becomes active when it detects a beta-lactams antibiotic, “says Zhou, an assistant professor in UConn’s Department of Pathobiology and Veterinary Science, who conducted the research with UConn pathobiologist Mazhar Khan and researchers in China. “It’s almost as if the antibiotic sets off an alarm bell and the protein leaps into action.”
The researchers don’t yet know the mechanism for this reaction, but now they know that this sensor exists, they will work on a way to disable it by developing drugs that can desensitize the bacteria – so that it doesn’t respond to the alarm.
“By combining new desensitizing drugs with existing antibiotics that are known to be effective,” says Zhou, “we can continue to use these tried and true drugs to combat disease.”
Zhou explains that over time, through mutation of their genetic material or other adaptations caused by repeated exposure to a particular antibiotic, bacteria can develop a resistance to antibiotics that have previously been effective.
This antibiotic resistance has reached a point where it is a public health concern across the globe. In fact, the Centers for Disease Control (CDC) put the number of people in the United States who become infected with antibiotic-resistant bacteria at some two million annually, with nearly 23,000 dying from previously treatable diseases.
The researchers have determined that this histidine kinase protein is widely present in all vibrio species, including V. cholerae, the organism responsible for cholera, an acute diarrheal infection that affects millions of people annually due to the consumption of tainted food or water. Administration of effective antibiotics can be an important part of the treatment protocol, especially in Third World countries where sanitation is often a problem.
There are many types of bacteria in addition to those in the vibrio family, however, and not all of them have the same type histidine kinase proteins. Further research into these bacteria is on the horizon, with the hoped-for result being new drugs that can outsmart the competition.