Researchers at UConn Health used stem cells derived from patients with Angelman syndrome to identify the underlying cellular defects that cause the rare neurogenetic disorder, an important step in the ongoing search for potential treatments for Angelman and a possible cure.
Up until now, scientists trying to understand why the brain cells of individuals with Angelman fail to develop properly have relied primarily on mouse models that mimic the disorder.
By using human stem cells that are genetically identical to the brain cells of Angelman syndrome patients, researchers now have a much clearer and more accurate picture of what is going wrong.
In a study appearing today in the journal Nature Communications, the researchers report that the brain cells of individuals with Angelman syndrome fail to properly mature, causing a cascade of other developmental deficits that result in Angelman syndrome.
“We looked at the electrical activity of these brain cells and their ability to form connections, which is critical to the working circuits in the brain,” says UConn Health neuroscientist Eric Levine, the study’s lead author.
“We found that the cells from Angelman patients had impairments,” says Levine. “They didn’t develop the same way as they do in people who don’t have the disorder. They failed to develop mature electrical activity and they didn’t form connections as readily.”
Angelman syndrome appears in one out of every 15,000 live births. People with Angelman have developmental delays, are prone to seizures, and can have trouble walking or balancing. They have limited speech, but generally present a happy demeanor, frequently laughing and smiling.
The disorder occurs when a single gene that individuals inherit from their mother’s 15th chromosome is deleted or inactive. The paternal copy of that gene, known as UBE3A, is normally silenced in brain cells.
The research study led by Levine was done in collaboration with another research team at UConn Health led by developmental geneticist Stormy Chamberlain. Chamberlain is investigating the underlying genetic mechanisms that cause Angelman and how they might be reversed. Levine’s research team meanwhile, is looking at the physiology behind the disorder or what happens in the brain when the maternal UBE3A gene is missing or fails to work properly.
“What’s interesting about this particular study is that Eric captured some of the first electrophysiological differences between Angelman syndrome neurons and typically developing neurons, and it appears those primary deficits are setting up all of the other problems that are happening downstream,” says Chamberlain.
The human brain relies on electrical signals to process information. These signals pass between the neurons in our brain via special connections called synapses. In the current study, Levine found that at about three to five weeks into their development, brain cells in unaffected individuals ramp up their electrical activity while cells from Angelman patients do not. That failure to mature disrupts the ability of the Angelman cells to form proper synaptic connections, which is critical for learning, memory, and cognitive development.
“Other researchers haven’t seen this deficit in mouse models but we think it might have something to do with where they were looking,” says Chamberlain, who is a co-author on the current study. “In the mouse studies, researchers have been looking at either adults, juvenile, or early postnatal neurons. Eric is looking at some of the earliest changes in neurons that likely occur during fetal development.”
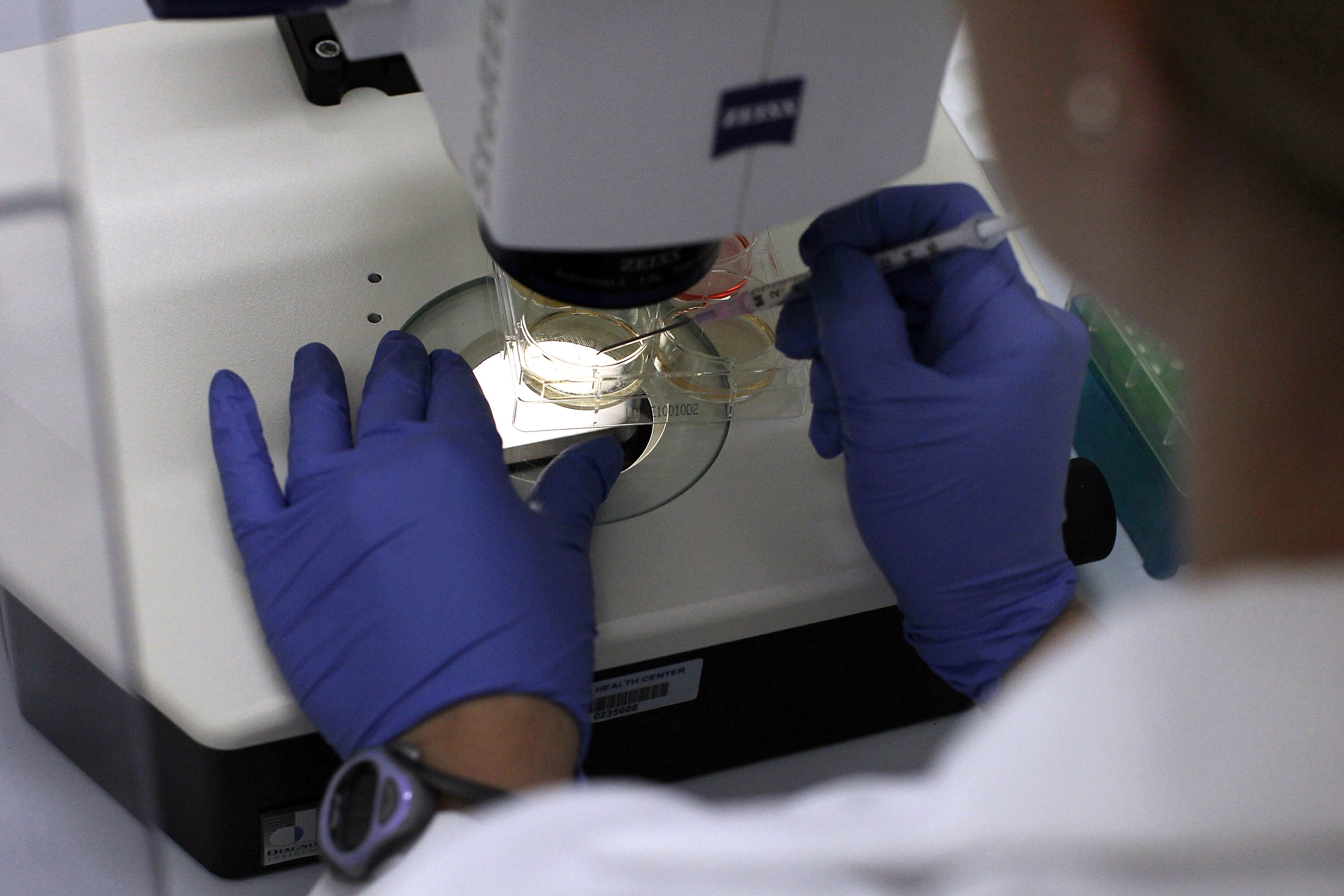
Angelman patients are very active in the ongoing research into the disorder. The induced pluripotent stem cells used in Levine’s research were derived from skin and blood cells donated by people with Angelman. Those cells were then reprogrammed into stem cells that were grown in the lab into brain cells that match the patient’s genetic makeup. This process allowed Levine to closely monitor how the cells developed from their very earliest stages in vitro and to see how they differed from control cells taken from people without the disorder.
To confirm that the cellular defects in the Angelman cells were caused by the loss of the UBE3A gene, Levine edited out the UBE3A gene in cells from the control group to see what would happen. Indeed, the same cascading chain of events occurred.
“In the control subjects who did not have Angelman, we basically knocked out the gene in order to mimic the Angelman defect,” Levine says. “If you do that early enough in development, you see all of the things go wrong in those cells. Interestingly, if you wait and knock out the gene later in development, you only see a subset of those deficits.”
Those results led Levine to believe that the delayed development of electrical activity in the brain cells from patients with Angelman is one of the driving factors causing other defects to occur. That knowledge is important for the development of possible drugs to combat Angelman. If scientists can stop that initial electrical failure from happening, it might prevent the other developmental problems from happening as well. Researchers with Ionis Pharmaceuticals from Carlsbad, California also participated in the current study.
With this new information in hand, Chamberlain and Levine are taking the research to the next level. They want to know exactly how the loss of the UBE3A gene causes the development of electrical activity in the early brain cells of Angelman patients to stop.
Another benefit of the current study is that the stem cell model created by Chamberlain and Levine can now be used to screen potential therapeutics for Angelman. Having the ability to monitor human brain cells in the lab will allow researchers to test dozens if not hundreds of compounds to see if they reverse Angelman’s cellular defects. The same process could be applied by scientists looking into other disorders.
And that’s good news.
“The Angelman Syndrome Foundation was proud to fund Dr. Levine’s research in 2011 and we are thrilled to see the results,” says Eileen Braun, executive director of the national nonprofit organization that funds Angelman syndrome research and supports individuals with Angelman and their families. “Having results published in Nature Communications, a prestigious, peer-reviewed journal, illustrates the validity of this research, which ultimately helps us understand more about Angelman syndrome and helps lead us to our ultimate goal of treatments and a cure.”
Individuals interested in supporting people with Angelman syndrome and Angelman research are welcome to participate in a walk supporting the Angelman Syndrome Foundation on May 20 at Northwest Park, 448 Tolland Turnpike, Manchester, Connecticut. Registration opens at 8:30 a.m. The walk beings at 10 a.m. Donations are encouraged and accepted. The University of Connecticut is a sponsor of the walk.