Take a deep breath and hold it. Keep holding it. Keep waiting … wait … don’t breathe yet … Feel that burning in your lungs?
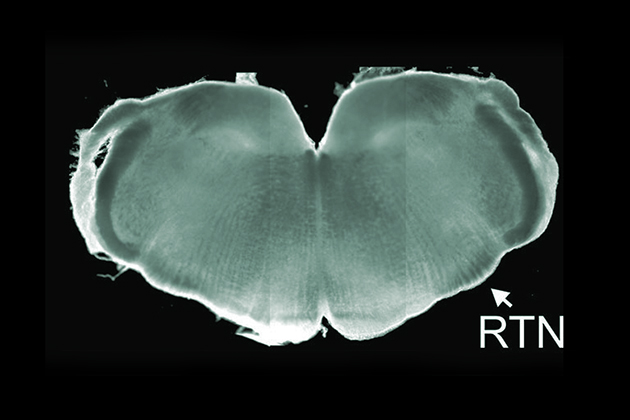
That’s your brain telling you to breathe. Or rather, that’s a tiny group of cells in the brain stem telling you to breathe. Those cells can sense the buildup of carbon dioxide in your blood, thanks in part to a protein called connexin. Carbon dioxide latches onto connexin, which then spurs cells to signal “it’s time to breathe!” Neurons fire, your diaphragm moves down, and you inhale.
Babies start breathing in the womb, inhaling and exhaling irregularly at first, and then gradually more and more, until the day when they’re born and have to do it all the time. But premature babies sometimes have trouble. They stop breathing periodically, sometimes for 20 or 30 seconds at a time. Sometimes they’re fine, and sometimes they’re not, and doctors struggle to help them.
That may soon change, however, thanks to a two-month-old patient at UConn Health with a rare connexin mutation, and his doctor’s willingness to call for help.

The patient was just two months old, deaf, blind, and covered in thick, leathery, cracked skin. And he had odd, disordered breathing that left his oxygen levels too low. He had been referred to UConn Health for his skin condition, but neonatal research director Naveed Hussain was startled by the baby’s breathing troubles. Premature babies often have trouble breathing, but two-month-olds rarely do.
Hussain began searching for information about the baby’s mutation, which was at a spot on the genome called connexin26. Related mutations are known to result in deafness, blindness, or skin trouble. But no one had ever reported disordered breathing, at least not in humans. So Hussain began reading about animals with connexin mutations. Which is how he discovered that Daniel Mulkey, a UConn associate professor of physiology and neurobiology, had looked at just this type of mutation-related breathing disruption in rats. Hoping that Mulkey might be able to suggest a therapy for the patient, Hussain picked up the phone.
Mulkey was intrigued. He knew that a common connexin mutation blocked expression of the protein altogether. Having one copy of that mutation is a common cause of inherited deafness; having two copies is lethal in utero. But Hussain’s patient had one normal copy, and one connexin26 mutation. So why was he in such bad shape?
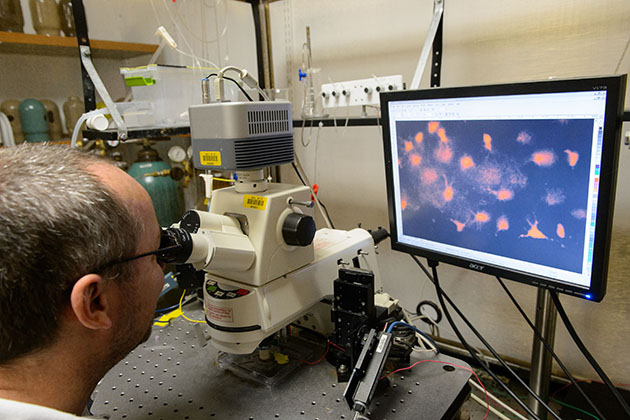
Mulkey asked Nick Dale, an expert on connexin protein at the University of Warwick, UK, to express the connexin26 mutation in human astrocytes. Astrocytes are the most abundant cells in the brain and do many things, including signaling to neurons. Dale found that astrocytes with the connexin26 mutation couldn’t bind to carbon dioxide. This specific connexin mutation was dominant, and suppressed expression of the normal protein. Such mutant cells were oblivious to dangerously high carbon dioxide levels, and this almost certainly explained the baby’s disordered breathing. It was also the first time a direct link between the connexin channel, carbon dioxide, and respiration had been shown in humans.
While Dale and Mulkey were looking at the mutation’s effect on human cells, Hussain began to review recordings of the breathing patterns of his patient, trying to see if there was anything that could give advance warning of a bad breathing episode. There’s not much in the medical literature about the breathing patterns of newborn infants, and Hussain and his colleagues began to wonder if they were even looking at the right things. He invited Mulkey and Xinnian Chen, a UConn assistant professor-in-residence in physiology and neurobiology who specializes in biosignal processing, to examine the recordings.
“They pointed out things we at the hospital hadn’t paid any attention to. We invited them to speak at one of our conferences, and that led to a discussion with fellows, and faculty questioning if we maybe could do more with breathing patterns in babies” to help them, Hussain says.
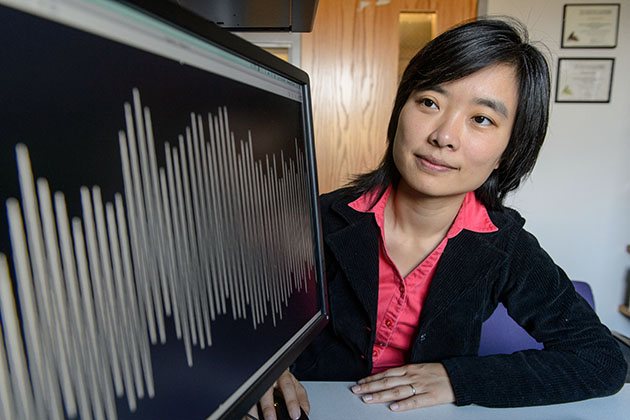
Chen began carefully sifting the data, looking at records of normal breathing, of bad breathing, and most importantly at the recordings taken minutes before the start of a bad breathing episode. She was searching for subtle differences that could serve as warning signs.
What she has found so far has been suggestive. It looks like healthy breathing rhythms are similar to healthy heartbeats. Both of them have slight blips and variations here and there. Heart rhythms have been studied extensively, and cardiologists know that if a heart starts to beat too simplistically regularly, a heart attack is likely in the coming hours. With Hussain’s help, the team is gathering recordings of many more premature infants and developing an algorithm that should eventually be able to pinpoint when a baby’s breathing pattern goes south.
Sadly, the findings couldn’t help Hussain’s patient, but the researchers hope their early warning system will be able to save other infants, alerting health care providers to dangerous breathing patterns before a baby gets into serious trouble.



