Dr. Lindsay Bliss, fresh out of the UConn School of Medicine and into a surgical residency at the UConn Health Center, is determined to improve the culture of the operating room to maximize patient safety.
An opportunity came along during her third year of medical school, while on her inpatient surgery experience at Saint Francis Hospital and Medical Center.
“It was during this rotation that I learned about Saint Francis’ involvement in the National Surgical Quality Improvement Program and met Dr. [Scott] Ellner,” she says. Ellner is an assistant professor of surgery at the UConn School of Medicine and is Saint Francis’ director of surgical quality.
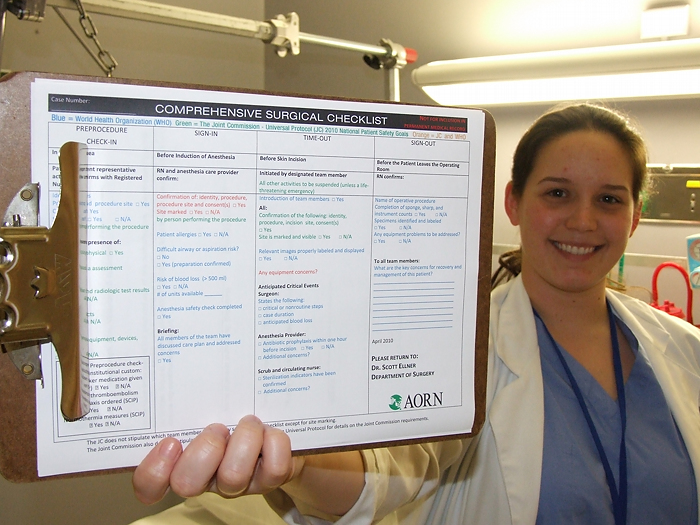
In a matter of months, Bliss had taken the student lead in a major OR patient safety project at Saint Francis. She would spend the next year collecting data in operating rooms for the project that would become known as “OR Team Training on the Use of a Surgical Checklist to Improve Patient Outcomes.”
“While most fourth-year medical students were winding down and looking forward to Match Day, Lindsay was spending 8 to 10 hours a day in the operating room observing cases on her own time,” Ellner says. “She is a star in the making.”
The initiative was to improve surgical outcomes by training OR staff on a standardized process with a surgical checklist.
“It was also focused on cultivating communication skills in order to optimize transfer of information and address disruptive, safety-compromising behavior,” Bliss says. “The idea was to observe behaviors in the OR and develop systems and strategies to improve them.”

Bliss observed about 100 cases to study the checklist’s impact on communications. The data indicate use of the checklist contributed to a decrease in infections and postoperative complications: overall 30-day morbidity went from 21 percent to less than 7 percent.
“Most importantly, this study used team training strategies to change the culture in the operating room,” Ellner says. “Forty one-hour sessions were given to the operating room staff, from circulating nurses, recovery room nurses, scrub technologists and pre-op nurses, on how to have difficult conversations with other team members when things are not always going as planned. For example, a scrub technologist would address a surgeon in a polite, non-confrontational manner if there was an incident that occurred in the OR”
Bliss is the lead author of the paper on the first phase of the checklist project. She’s presented the data to the Florida State Surgical Collaborative and given a poster presentation at the American College of Surgeons NSQIP Meeting in Boston.
Bliss’ efforts earned her a Patient Safety Leadership Scholarship from the Saint Francis Department of Surgery. The scholarship was started with a donation from one of Ellner’s patients, who wanted it to go toward patient safety and quality initiatives.
“The intention was to educate students and future leaders in health care,” Ellner says. “The scholarship is a leadership fund for patient safety. Lindsay leads by example.”
“It’s an incredible honor,” she says. “It’s nice for a gift from a patient to be used to refocus on patient safety and on getting medical students aware of patient safety. It’s really important to train future generation of surgeons and clinicians in general to recognize patient safety issues and become advocates for patients.”
Before graduating this spring, Bliss was among a group of UConn medical students who attended the second annual National Women in Surgery Career Symposium at the University of South Florida in Clearwater.
Bliss’ work on the surgical safety checklist project represents the start of ongoing research to improve patient safety in the OR.
“This was a preliminary study and there is much more work to be done,” Ellner says. “The next phase will be engaging the surgeons and anesthesiologists for this project.”