A new blood test could help doctors identify patients at risk for delirium, a sudden, acute state of confusion that most often affects older adults and incurs $6.9 billion in medical costs each year in the U.S. It comes on quickly and can signal serious health trouble.
Despite the dangers, hospital staff are not always on the lookout for delirium because it can be difficult to recognize. But researchers at the University of Connecticut (UConn Health) and Beth Israel Deaconess Medical Center have found that a blood test could make it easier to identify patients at risk. Their study, published online in the Journal of Gerontology: Medical Sciences, reports that elevated blood levels of specific proteins, called cytokines, can hint that a patient will develop delirium during a hospital stay.
“We’re beginning to uncover a blood signature associated with delirium,” says George Kuchel, director of the Center for Aging at UConn Health and one of the authors of the study. That blood signature shows two cytokines at higher than normal levels in patients who develop delirium. Both cytokines are associated with inflammation, the redness, swelling, heat, and pain associated with injury and irritation.
“We often think of infections as causing inflammation, but anything that causes tissue injury can cause inflammation,” explains Edward Marcantonio, director of the Aging Research Program at Beth Israel Deaconess Medical Center and a professor of medicine at Harvard Medical School. Marcantonio and colleagues at Beth Israel were co-authors of the study. “Surgery is also an inflammatory stimulus.”
Inflammation and delirium seem to be linked, although researchers don’t yet know exactly how. The two cytokines the researchers saw in the blood signature, interleukin-6 and interleukin-2, can cause swelling of the membrane around the brain. Chronic stress from low-level illness can also elevate both cytokines and stress hormones such as cortisol, which over the long term can shrink part of the brain and perhaps increase an elderly person’s susceptibility to delirium.
Delirium often begins a cascade of negative events that culminate in a loss of independence and increased chance of sickness and death. Nearly half of older adults who undergo hip or knee replacement or open heart surgery will become delirious in the hospital, increasing hospital stays, re-admission, and the need for intensive care. Patients who develop delirium in the hospital still have cognitive problems up to one year later, and have increased risk of dementia long term.
A new technique for measuring biomarkers
To get a better handle on the relationship between inflammation and delirium, Kuchel, Marcantonio, and their colleagues worked with 566 patients who participated in SAGES (Successful Aging after Elective Surgery Study). This large study sponsored by the National Institute on Aging has been following 566 surgical patients over the age of 70 for the past five years, with the goal of finding new approaches to prevent delirium and its long-term consequences in older adults.
Marcantonio and the other researchers at Beth Israel Deaconess Medical Center worked directly with the patients. They wanted to test the patient’s inflammatory biomarkers several times before and after surgery to get a more complete picture of how inflammation correlated with delirium. But the existing methods required too much blood and could only measure one biomarker at a time. Other blood assays were commercially available that could test more than one, but they didn’t work very well with the blood of the elderly, which tends to be more viscous than the blood of younger people.
“The bottom line is that we needed to evaluate networks of different inflammatory pathways,” says Kuchel, “and that could only be accomplished by measuring multiple cytokines at a time.” Kuchel and his colleagues adapted and optimized for use in the elderly a customized technique that could measure 12 inflammatory biomarkers using very little blood.
The researchers then assessed and compared the biomarkers of the SAGES patients, looking for differences between delirium cases and no-delirium controls. The spike in interleukin-6 in the two days after surgery stood out immediately. Further analysis showed that patients who developed delirium had higher levels of interleukin-2 than non-delirium patients at all the times they were tested, both before surgery, in the first two days afterwards, and then one month later.
This is the first study to look at cytokine levels in older surgical patients at several points in time, both before and after surgery. The results need to be replicated in other studies, but if they prove to be generally true, the blood signature could provide a quick way to alert doctors and nurses to seniors at higher risk of delirium. They can then take extra precautions to keep the patients oriented.
“Lots of possible interventions can help prevent delirium,” says Kuchel. “For example, if you do things such as improve a patient’s vision and hearing, reorient them to where they are regularly, promote restful sleep, increase mobility, and stop medications that could be making the delirium worse, all these things can help.”
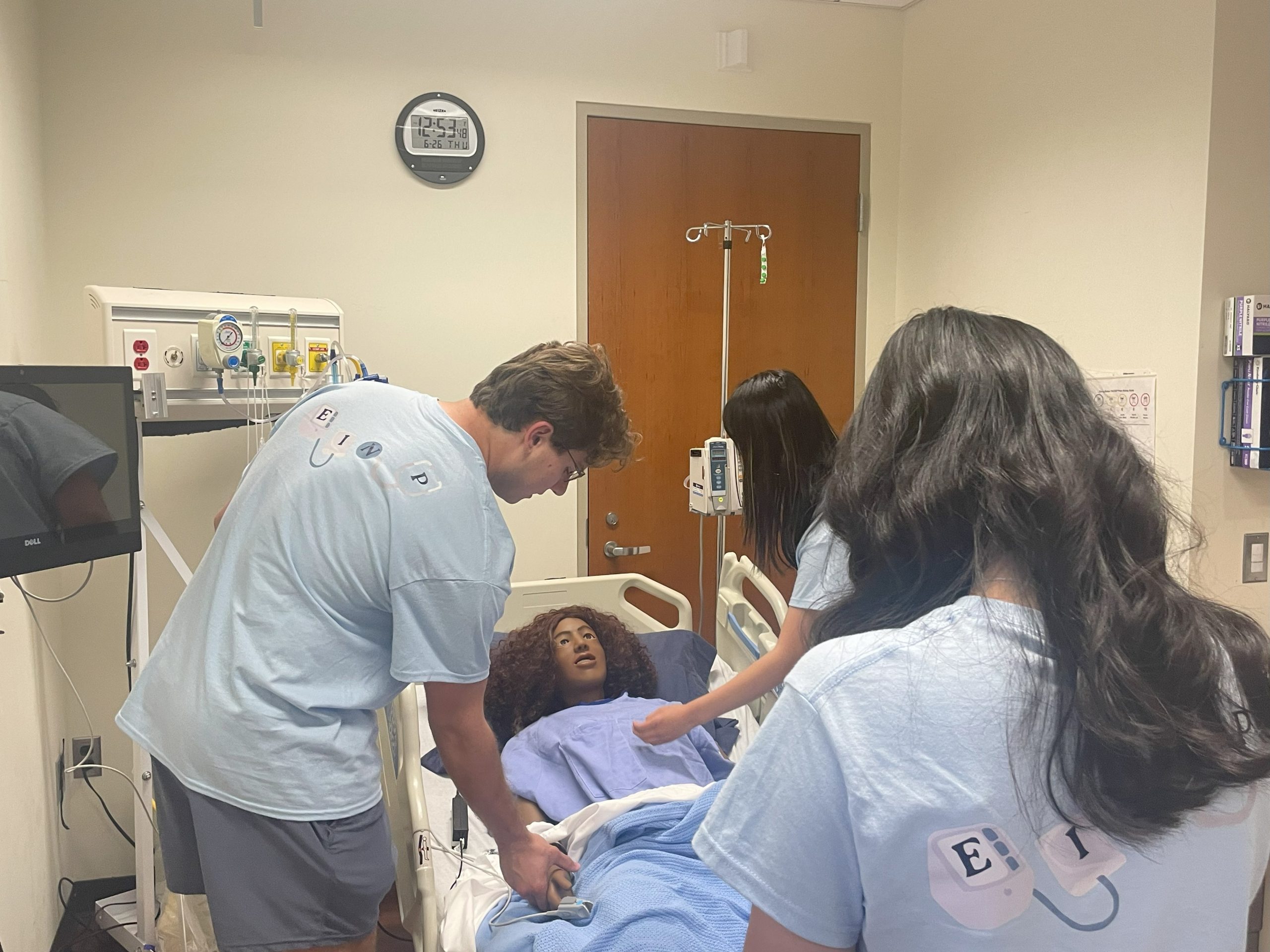
As part of UConn Health’s work to detect and prevent delirium and improve the care of older patients, geriatrician Laverne Wright and hospitalist Nicole Silverstein are testing better ways to detect delirium in hospitalized patients.
Study results were recently presented at the Alzheimer’s Association International Conference in Washington, D.C., on July 21.
This study was supported by the following grants from the National Institute on Aging: T32AG023480, PO1AG031720, K07AG041835, R01AG030618, K24AG035075.