UConn Health has begun tracking cancer patients with an advanced heart imaging test before, during, and after chemotherapy and radiation therapy care, with the goal of detecting any potential cardiac health risks or conditions early.
There are currently more than 15 million cancer survivors in the U.S., and that number is expected to grow to 20 million within 10 years. But as more patients survive cancer, the potential risk of developing cardiovascular health issues from lifesaving chemotherapy and radiation treatments is also increasing.
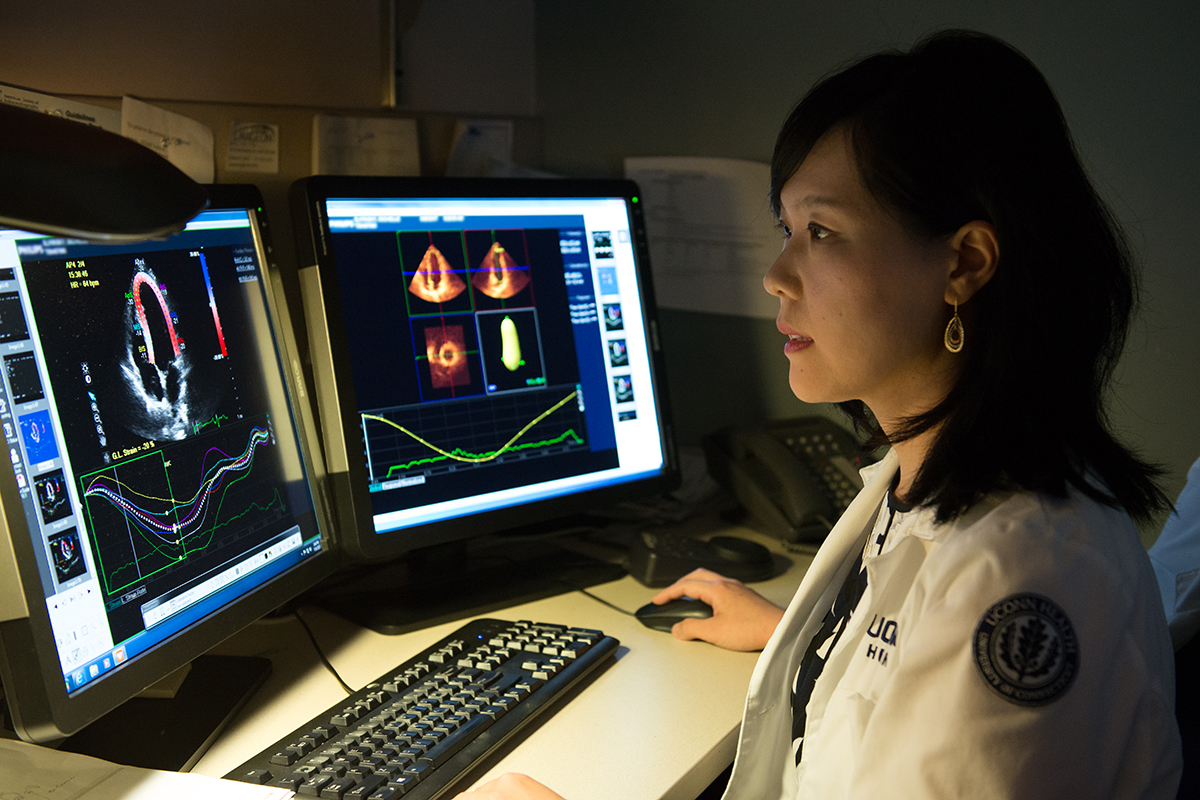
New echocardiography strain imaging is now allowing cardiologists to hunt for any early warning signs of heart muscle function changes or damage within the heart tissue’s tiny speckles. The in-depth strain analysis is powered by traditional ultrasound technology, which uses high-frequency soundwaves to create a sonogram of the pumping heart.
Echo strain imaging has been compared to a canary in the coal mine. — Dr. Agnes Kim
On a subclinical level, before any symptoms even present, echo strain imaging allows a cardiologist to identify any potential impact of cancer treatment on the heart’s left ventricular function, the thickest heart chamber, that controls the pumping of oxygenated blood throughout the body. If the left ventricle does not function well, it can lead to heart failure.
Dr. Agnes Kim, director of the Cardio-Oncology Program at the Calhoun Cardiology Center at UConn Health, says it’s very important to monitor cancer care patients for any signs of cardiac toxicity. “Echo strain imaging has been compared to a canary in the coal mine,” she says. “We are so grateful that our cancer patients have access to this latest technology so that we can monitor and intervene early on if any warning signs are present.”
The risk of cancer care side effects showing up during treatment or years down the road is a big concern of cardio-oncology specialists like Kim. That’s why she launched the program in 2014.
Kim says it is key that UConn Health has an integrated program of oncologists and cardiologists, which allows for coordinated care to address the potential risks to heart health that can arise from cancer treatment.
Research studies have shown that confirming any changes in heart muscle strain can help doctors predict whether a patient is at risk for cardiotoxicity and its side effect of developing heart failure in the future. If a patient is found to have a 15 percent or more decline in heart strain, it is suggestive of cardiotoxicity, and doctors may prescribe cardio-protective drugs, such as a beta-blocker or ACE inhibitor, or modify the patient’s chemotherapy dosage.
Possible cardiotoxicity side effects from chemotherapy medications include a lowering of overall heart muscle function, which can lead to heart failure, formation of blood clots, or an increase in blood pressure. The side effects of radiation therapy can also lead to damaged heart muscle, heart valves, and arteries, or impact the lining of the heart.
In hopes of gaining further insights, this program is currently studying the use of echo strain imaging, and also the presence of serum biomarkers in the blood for predicting whether a cancer patient is at high risk for cardiotoxicity. The program is also tracking cancer patients’ long-term heart health, to analyze the impact of additional clinical care protections.
Patients receiving such chemotherapies as doxorubicin (Adriamycin), trastuzumab (Herceptin), bevacizumab (Avastin), and 5-FU may be more at risk for cardiotoxicity. The majority of these chemotherapies are used to treat breast, gastrointestinal, and lymphoma or leukemia cancer patients.
Kim says every cancer patient should talk to their oncologist about the potential side effects of their cancer treatment plan and how to reduce any heart health risks during and after cancer care.
To learn more about the Cardio-Oncology Program at UConn Health, visit this website or call: 860-679-3343.