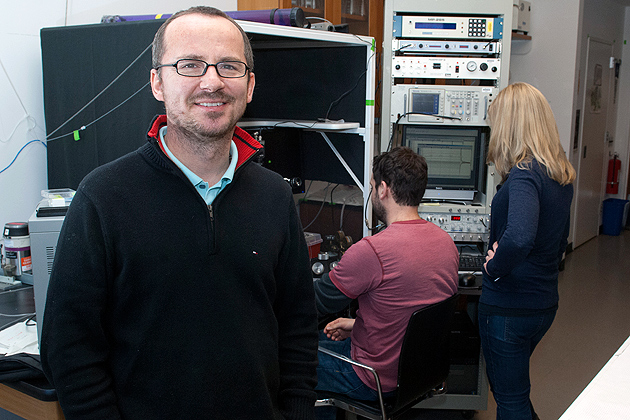
Professor Daniel Mulkey from the University of Connecticut Department of Physiology and Neurobiology recently received several grants for projects that focus on understanding how the brain controls breathing in health and disease.
The first project is titled “Role of KCNQ2 Channels in Control of Breathing” (Award #: HL1377094). Mulkey and co-PI Anastasios (Tasso) Tzingounis, an associate professor in the UConn Department of Physiology and Neurobiology, received nearly $1.7 million from the NIH/National Heart, Lung and Blood Institute to study how mutations in a type of potassium channel called KCNQ affects breathing. Clinical evidence has identified loss- and gain-of-function mutations in KCNQ channels (namely the KCNQ2 channel) in patients with severe forms of early onset epileptic encephalopathy, a key symptom of which is abnormally suppressed breathing. The mechanism(s) by which KCNQ2 channel variants cause respiratory dysfunction are completely unknown.
To test this, the researchers will genetically engineer mice to express human KCNQ2 mutations in order to determine how expression of these mutant channels affects cellular excitability, respiratory neural network function and respiratory behavior. By understanding whether and how KCNQ2 channels regulate the activity of specific subsets of respiratory neurons, this work will lay a foundation for developing treatments for respiratory problems associated with epileptic encephalopathy.
Mulkey was recently funded by the Dravet Foundation for a project titled “Disordered breathing contributes to SUDEP in a mouse model of Dravet syndrome.” The $150,000 award will fund work to identify mechanisms contributing to respiratory dysfunction in Dravet syndrome (DS), is a severe form of neonatal epilepsy with a high mortality. A leading cause of death in patients with epilepsy is respiratory failure. Despite this, little is known regarding how control of breathing is disrupted in epilepsy. Therefore, there is an urgent need to determine whether DS-associated gene mutations disrupt breathing and contribute to death in DS. To test this, Fu-Shan Kuo, a graduate student and American Epilepsy Society fellow in the Mulkey lab, will introduce a human DS mutation into respiratory neurons in mice and characterize respiratory function at the cellular, network and whole animal levels. Results of this work will yield the first mechanistic insight into the cause of respiratory failure in DS.
Finally, Mulkey recently renewed a grant from the NIH/National Heart, Lung and Blood Institute (“Glial chemosensitivity and control of breathing in Rett syndrome” HL104101) to investigate the role of astrocytes in control of breathing. This project is part of a collaboration with Michelle Olsen, Ph.D., a researcher from Virginia Tech. In conjunction with the previous five year cycle, this award total is over $2.6 million.
The goal of this project is to determine the contribution of astrocyte Kir4.1 channels to respiratory dysfunction in Rett syndrome (RTT), a condition characterized by mental disability, autistic behavior, seizures and profound respiratory problems. RTT is caused by loss-of-function mutations in the gene encoding methyl-CpG-binding protein 2 (MeCP2). Previous work shows that astrocytes contribute to respiratory drive by sensing changes in CO2/H+ via inhibition of a potassium channel known as Kir4.1. Preliminary evidence suggests that MeCP2 regulates expression of Kir4.1. Therefore, the researchers are testing the hypothesis that MeCP2 deficiency compromises Kir4.1 channel expression, and thus the contribution of astrocytes to the control of breathing.
The Mulkey lab is one of few labs in the world studying neural-astrocyte contributions to control of breathing under normal and diseased conditions. According to Mulkey, this work is also made possible by the help of outstanding collaborators and the supportive environment of the Department of Physiology and Neurobiology at UConn.
Mulkey received his Ph.D. from Wright State University. He uses a combination of slice-patch electrophysiology, fluorescent imaging and genetic approaches to identify ion channels that regulate activity and neurotransmitter modulation of respiratory neurons. His lab also uses similar approaches to explore how astrocytes sense environmental cues and communicate with neurons and vasculature to fine tune respiratory output.
Anastasios (Tasso) Tzingounis received his Ph.D. from the Vollum Institute. His laboratory addresses questions related to molecular and cellular neuroscience using a combination of approaches including mouse genetics, electrophysiology and microscopy.