University of Connecticut and University of California-Davis researchers announced in the Proceedings of the National Academy of Sciences on Sept. 25 a breakthrough in understanding which cells protect against Salmonella infection – a critical step in developing a more effective and safe vaccine against a bacterium that annually kills an estimated one million people worldwide.
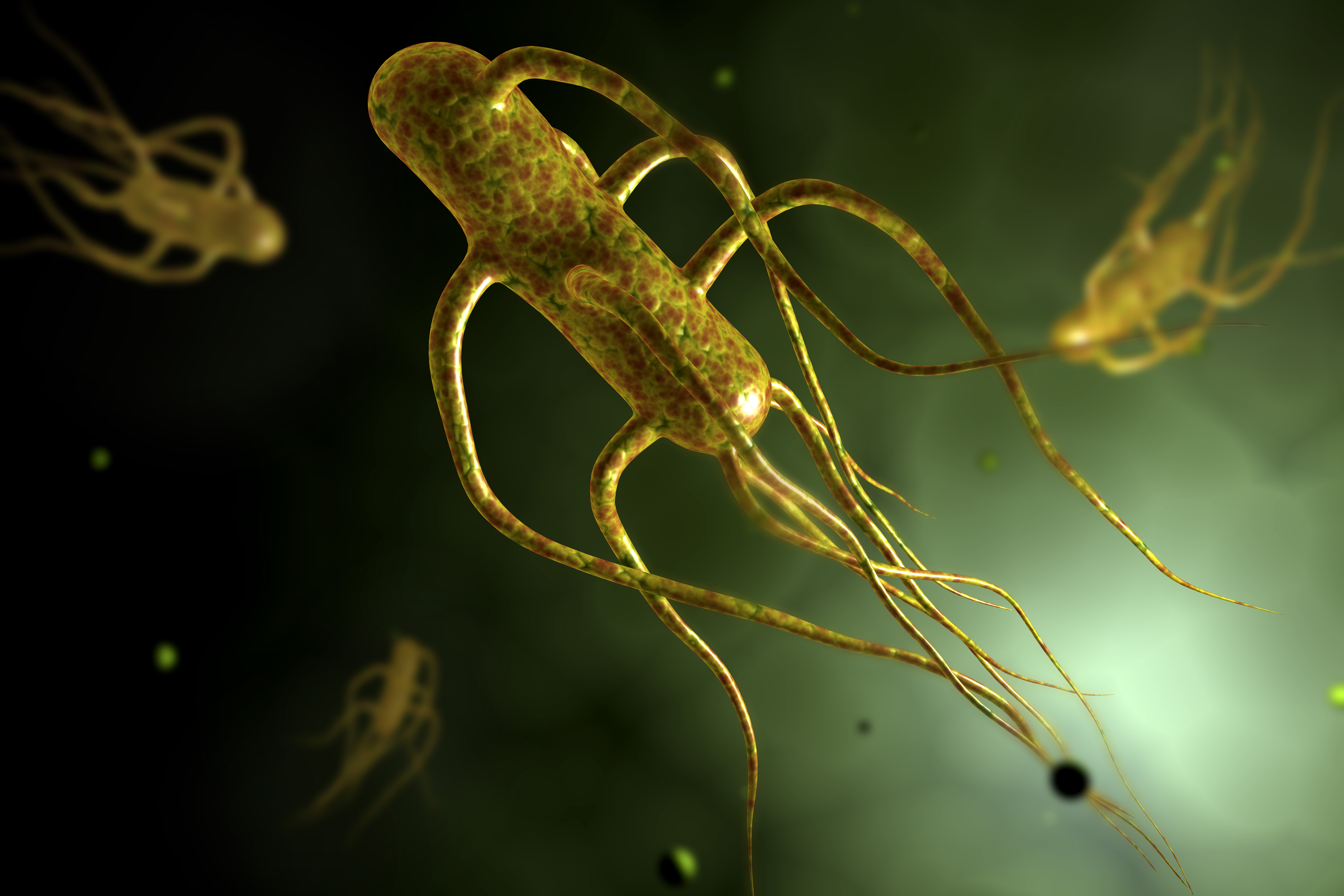
Salmonella typhi causes life-threatening enteric fever (historically called typhoid fever), commonly in Africa and parts of Asia. Other strains of Salmonella are capable of causing gastroenteritis or invasive non-typhoidal Salmonellosis (NTS), an emerging disease in sub-Saharan Africa. Enteric fever and NTS can be fatal in 20 to 25 percent of infected individuals without access to medical care.
There are two vaccines currently available for Salmonella, but neither are practical for use in sub-Saharan Africa and they only protect about 50 percent of people immunized.
What hasn’t been realized until very recently is there are actually two different categories of T cells – those that circulate through tissues in the body and those that never move. — Stephen McSorley
A collaborative group of scientists from the University of Melbourne, Australia, UConn Health, and the University of California-Davis decided to investigate how the vaccines work, in order to understand how they could be improved. They focused on a relatively unknown type of immune cell, called non-circulating memory T cells. Memory T cells are long-lived and are the immune system’s recall mechanism. When they re-encounter a bacteria, virus, or other pathogen they’ve seen before, they quickly multiply and alert the rest of the immune system to the invasion.
“What everyone has been focused on in immunology – not just in addressing Salmonella, but all infectious diseases for the past 50 years or so – has been antibody and T cell responses,” said Stephen McSorley, lead author and interim director of the Center for Comparative Medicine at UC Davis. “What hasn’t been realized until very recently is there are actually two different categories of T cells – those that circulate through tissues in the body and those that never move and are known as tissue-resident or non-circulating memory cells.”
Since non-circulating memory T cells were discovered, McSorley said, there’s been a rush in different disease models to understand whether they are important or not – in cancer and infectious diseases. It seems in some models they are very important; in others, they are less so.
During the study, graduate students from UC Davis made several trips to UConn to conduct experiments in collaboration with UConn immunologist Lynn Puddington and her team, experts in the definitive approach to distinguish circulating versus resident cells. The technique involves connecting and then disconnecting the circulatory systems of unrelated mice. One mouse in each pair had been vaccinated against Salmonella; the other mouse had not. Thanks to fluorescent markers, the team was able to show that the T cells that protected against Salmonella infection lived in the vaccinated mouse’s liver, and stayed there. They never made it to the unvaccinated mouse’s liver. These cells were obviously non-circulating T cells.
“This evidence that non-circulating T cells play a key role in protection from this major pathogen is really exciting,” says Puddington. Generating these cells may be the basis of future vaccines against typhoid and NTS.
Current Salmonella vaccines limited
Non-typhoidal Salmonellosis has really emerged in Africa in the past 10 years, mainly in young children, the elderly, and HIV positive individuals – basically, people with compromised immune systems. They get a strain that would normally cause stomach upset, but in these individuals, it causes systemic infection and can kill them.
“The goal of our lab is to understand the mechanisms of protective immunity in mice to learn tricks of the immune system, and then develop a vaccine that could replicate that to use for kids and people who live in these areas,” UC Davis’s McSorley said. “We found that you absolutely need these non-circulating T cells to protect against Salmonella. That’s an important milestone, because if you’re going to make a vaccine, you have to know what you’re trying to induce with that vaccine. Now that we know these forms of T cells exist and protect against Salmonella, the next goal is to try to develop synthetic ways to induce them to make a vaccine.”
McSorley said they have some ideas about how to do that, and that’s where the next phase of their research is going – to try and take vaccine components in a mouse model to focus specifically on these non-circulating cells and see if they can induce them.
“If we can learn how to better induce them and if we can apply that to a new Salmonella vaccine,” he said, “it should be more efficient at providing immunity than previous vaccines.”
Co-authors include Joseph Benoun, Oanh Pham, Victoria Rudisill, and Zachary Fogassy from UC Davis’s School of Veterinary Medicine; Newton Peres, Nancy Wang, Paul Whitney, Daniel Fernandez-Ruiz, Thomas Gebhardt, Sammy Bedoui, and Richard Strugnell from the University of Melbourne; and Quynh-Mai Pham and Lynn Puddington from UConn Health.
This study was supported by grants from the NIH’s National Institute of Allergy and Infectious Diseases and the National Health and Medical Research Council of Australia.
Trina Wood is a communications officer for the UC Davis School of Veterinary Medicine. Twitter: @ucdavisvetmed