Surgeons at UConn Health have a new option for minimally invasive procedures.
The da Vinci Xi System expands on the core features of earlier robotic surgery systems, offering even greater access, vision, and precision when performing robot-assisted procedures.
“The Xi gives us the ability to do multi-quadrant surgery,” says Dr. Eric Girard, one of the UConn Health surgeons who uses the new system. “What this means is it allows for a faster more efficient way to do the surgery than is already being done by the previous robot. It also allows us to expand what we can offer as a minimally invasive surgery. I can now take out an entire colon and rectum robotically, whereas before, I would not offer patients this procedure on the old robot.”
One example of a procedure where minimally invasive surgery historically was not an option is bowel anastomosis, in which the surgeon essentially splices the large intestine back together after removing a section of it.
“I can anastomose [splice] two ends of a bowel together inside the body with ease instead of making large incisions and doing it outside the body,” Girard says. “This translates to people feeling better faster and getting back to their families and their jobs sooner. I have had patients home within one day where the national average is five days.”
Dr. Ben Ristau, UConn Health’s surgical director of urologic oncology, says the updated instrumentation enables him to offer wider range of procedures, including robotic prostate removal for prostate cancer, removal of a kidney tumor while leaving the healthy kidney behind, or a partial nephrectomy (partial kidney removal), and robotic bladder removal for bladder cancer.

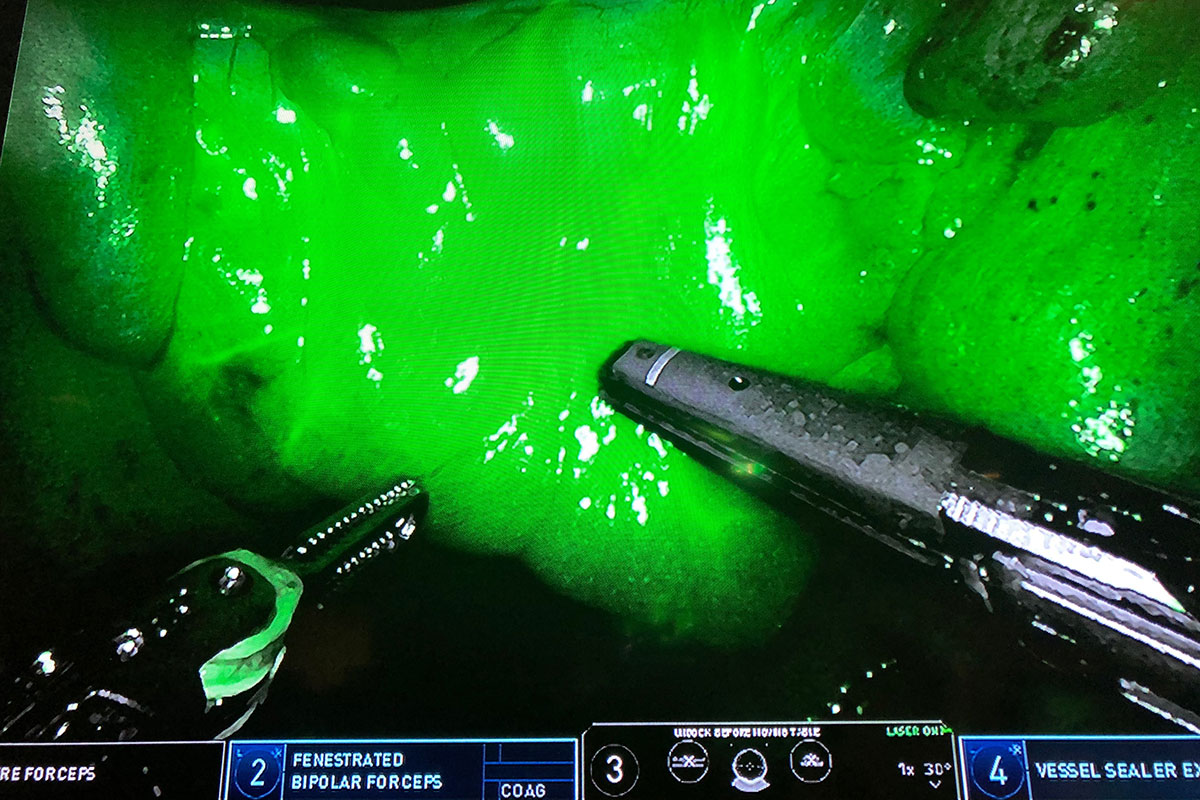
An advanced endoscope provides a highly magnified, 3D, high-definition view, virtually extending the surgeon’s eyes and hands into the patient. Surgeons also have a greater range of anatomical access, motion, and reach.
“We can adjust the patient’s position with the robot docked to the patient,” Ristau says. “This allows for greater access to both the abdomen and the pelvis and translates into a faster minimally invasive operation.”
Primary functions at UConn Health are in general, urologic, colorectal, and gynecologic surgeries.
It’s also a more effective training tool than its predecessors, according to Dr. Brian Shames, UConn Health general surgeon with expertise in minimally invasive and hepatobiliary procedures (those having to do with the liver, the gallbladder, bile ducts, or bile).
“The training modules are much more realistic,” Shames says, “and provide better simulation of actual operations, including hernia repair.”



