Becky Riendeau, of Unionville, is celebrating her 68th birthday this week thanks to the lifesaving vascular surgery care she received at UConn John Dempsey Hospital by Dr. Kwame Amankwah and his vascular surgery team.

After three visits to the Emergency Department for an upper respiratory infection and cough that just wouldn’t go away, a CT scan incidentally revealed a major, life-threatening condition lurking deep inside her body known as an aortic dissection.
“The imaging scan showed a split in my thoracic and abdominal aorta,” says Riendeau. “I am so lucky it was found. If I didn’t have that scan, I would never have known it was there nor what could have ultimately happened to me at any moment.”
Riendeau adds: “Never in a million years did I think this would ever happen to me. Maybe potentially get hit by a bus, but never did I think an aortic dissection was ever in my life’s playbook.”
The aorta is a major artery, the largest in the body, delivering oxygen-rich blood from the heart down through the abdomen. The aorta actually has three distinct layers of tissue. If one of its inner layers weakens or tears it can cause them to become dissected or separated.
“When an aortic dissection occurs the aorta can get bigger, start leaking blood and eventually rupture,” stresses Amankwah, the new chief of vascular surgery at UConn Health who performed Riendeau’s successful and innovative aortic repair on June 18. “The condition can be deadly if left undiagnosed or not treated promptly.”
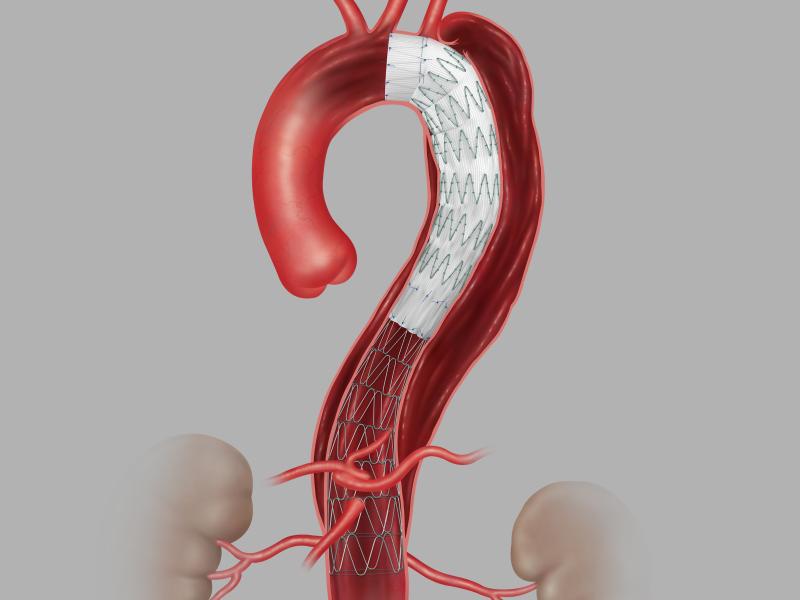
Thanks to Amankwah’s recent arrival to UConn Health and his advanced surgical expertise, Riendeau was the first patient at UConn Health and the second patient in the state to be treated surgically for an aortic dissection using a new aortic stent graft technology specifically designed for aortic dissections. The graft, made by Cook Medical, is known as the Zenith Aortic Dissection Graft. The aortic stent graft was approved by the FDA in February.
The aortic stent graft is placed through a small 1-centimeter incision through the skin into the artery in the patient’s groin. The aortic stent graft is then guided up the aortic artery under live x-ray imaging via a catheter to be fully expanded and deployed to replace the torn aortic lining. The new liner helps redirect and restore proper blood flow through the aorta and the body.

“The graft repair technology works seamlessly like replacing a broken pipe during a water main break but without the major digging,” says Amankwah. “The minimally invasive intervention is lifesaving – and beneficial to a patient’s more rapid recovery and healing since they are usually home from the hospital within 24 to 48 hours post-surgery.”
Amankwah recently placed one of the first Zenith devices in the country in a patient when previously at the State University of New York in Syracuse shortly before joining UConn Health.
According to Amankwah aortic dissections can at times be caught randomly through imaging tests when patients don’t present with any symptoms. However, warning signs of a potential aortic dissection can include uncontrollable high blood pressure and chest pain that radiates from the chest to the back. Sometimes this severe chest or abdominal pain can be mistaken for bad indigestion.
Amankwah stresses that patients like Riendeau with the major risk factor of uncontrolled high blood pressure need to see their doctor to have it corrected and closely managed. Also, if you have an aortic dissection discovered you must see a vascular surgeon immediately for close surveillance.
“Our vascular surgery program and team at UConn Health is great and growing,” says Amankwah. “It’s exciting to be here at UConn Health and we are committed to bringing the latest technology and vascular surgery techniques to the state and its citizens.”
Days after surgery Riendeau is already back to doing what she loves.
“I’m hugging my granddaughter again,” says Riendeau. “It’s remarkable to feel this good already and so much better than I expected. Along with restoration of my body’s proper blood flow, thanks to my aortic repair my quality of life has definitely been restored too.”
Riendeau is now able to enjoy the walks she loves with her husband more: “I am walking further today than I did before my surgery. With our recent retirements we now have big plans to look forward to.”
She also has a lot of praise for UConn Health’s lifesaving vascular surgery care.
“It was great. The doctors and nurses are fabulous at UConn Health. They are really special people,” says Riendeau, who shares a heartfelt thanks to all her nurses who cared for her across the ICU and surgical floors at UConn John Dempsey Hospital including Ted, Joy, Tanya, Jessica, Rachel, Tim, Effie, and Justina.