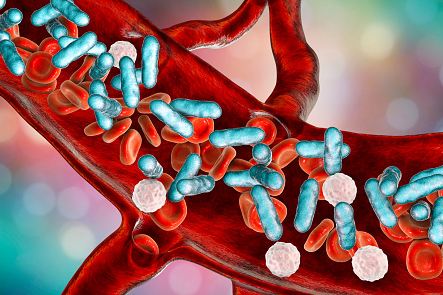
Sepsis is a relatively common – and dangerous – condition in which the body’s response to infection results in injury to tissues and vital organs. If unrecognized or untreated it can lead to shock and even death. Worldwide estimates are that up to 30 million people a year develop sepsis and up to 9 million people die each year from sepsis, and those who survive often have long-term consequences that impact their health and function.
The medical community recognizes Sept. 13 as World Sepsis Day, the goal of which is to raise awareness to this important clinical and public health topic. Dr. David Banach, UConn Health infectious diseases physician and hospital epidemiologist at the UConn John Dempsey Hospital, explains.
What might cause our immune system to harm – rather than protect – us?
The immune system is activated in response to an infection of the body and the purpose of the immune system activation is to kill the organism (usually a bacteria or virus) that is causing the infection. However, as a result of the infection and this associated immune activation and the impact this process has on the key organs such as the heart, blood vessels and lungs, patients with sepsis can become quite ill.
How preventable/manageable is sepsis?
Sepsis can often be avoided through measures to prevent infection, such as good hygiene practices and receiving recommended vaccinations. For patients who develop sepsis, early recognition and the appropriate treatment with antibiotics, controlling the source of infection and other supportive care interventions are essential in ensuring a good outcome.
Who is most prone to sepsis?
Anyone can develop sepsis but those who are at highest risk are very young, elderly and those who have chronic medical conditions, especially those which impact the immune system.
What are signs/symptoms?
Fever is the most common symptom associated with sepsis but other symptoms may also occur, including shaking chills, rapid heart rate, confusion, difficulty breathing, skin changes or mottling and a significant decrease in urination. While some who develop these symptoms may have sepsis, many will have other explanations, so prompt evaluation by a clinician is recommended if these signs and symptoms occur.
How is UConn Health dealing with sepsis?
UConn Health has a sepsis task force, a multidisciplinary team tasked with leading sepsis prevention, recognition and treatment efforts at UConn Health. The members include physicians, nurses, pharmacists, experts from the clinical laboratory as well as administrative leadership who help coordinate sepsis-related activities to ensure we are providing the highest quality of care for our patients with sepsis. Several members of UConn’s sepsis task force are also a part of statewide initiatives to improve sepsis care across Connecticut.
How much of a concern is antibiotic resistance with sepsis?
Given that most episodes of sepsis are caused by bacteria and antibiotic resistance among bacteria is becoming increasingly common throughout the world, antibiotic resistance is a significant concern. Unfortunately, we are seeing increases in the rates of sepsis caused by some antibiotic-resistant organisms. At UConn Health, through our infection prevention and control program and optimizing antibiotic use through antibiotic stewardship activities, we are working toward reducing the risk of antibiotic-resistant infections among our patients.
Learn more about infectious disease prevention and treatment at UConn Health.