If more than 7 million Americans have undiagnosed diabetes and another 76 million unknowingly have prediabetes, it adds up to roughly one in three of us being on a potential path to heart disease, stroke, kidney disease, vision loss, or amputation.
The numbers are based on estimates from the Centers for Disease Control and Prevention, and in many cases, these complications are preventable with better awareness and self-care.
As the name suggests, prediabetes is a precursor to adult onset, or type 2, diabetes. It’s when blood sugar levels are higher than normal and trending toward a diabetes diagnosis. More than half of type 2 diabetes cases are preventable with lifestyle choices.
“Our goal is to get people diagnosed with prediabetes sooner,” says Jean Kostak, one of UConn Health’s diabetes care and education specialists. “People who have prediabetes don’t know it because they haven’t been to the doctor, or because they may dismiss symptoms like hunger, thirst, frequent urination and feeling tired as normal signs of aging.”
In addition to increasing the risk of type 2 diabetes, prediabetes itself can be a risk factor for heart disease and stroke.
The International Diabetes Federation and the World Health Organization designate Nov. 14 as World Diabetes Day, on the birthday of Sir Frederick Banting, one of the discoverers of insulin. The theme this year is “Family and Diabetes.”
Family is a big part of both diabetes prevention and management. A family history of diabetes, along with obesity and being 40 or older, are the primary risk factors for type 2 diabetes.
And in the case of Millie Apanovitch, it was her family – her husband – who saved her from an acute episode in the emergency room 38 years ago.
“It was my husband who told me to get checked out because I was drinking more, I was waking up to urinate, and remember, I was in my early 20s,” Apanovitch says. “And my drink of choice was orange juice. He said, ‘I think you need to go to the doctor, I think you have diabetes,’ and the reason he said that was, his mother had diabetes. He knew the signs from his mother.”
Apanovtich has type 1 diabetes, in which the body can’t make insulin.
“Type 1 symptoms often present quickly,” Kostak says. “Type 1 is an autoimmune disorder where our own immune systems destroy the beta cells in the pancreas that make insulin. Therefore, insulin needs to be injected to assist the blood sugar to get into our cells so we can use it for energy. Type 2 is more gradual, in which a function of the pancreas to make insulin isn’t happening correctly. It’s either not making enough or there’s a lot of insulin resistance, meaning there’s insulin but the body’s not able to use it. Typically it’s because people are overweight.”
Apanovitch, who lives in Wethersfield, had to get into the habit of regularly checking her blood sugar and injecting herself with insulin to stay in a healthy range. For nearly 35 years it was one combination or another of finger pricks, chem strips, syringes and pens. Then about five years ago she switched to an insulin pump. The one she has today is about half the size of a smart phone and her clothing conceals it.
“This to me as far as I’m concerned helps me stay alive, helps me stay active, and I think it’s much, much easier and convenient,” Apanovitch says. “This one has a little pod that you stick on your stomach or on your arm, no needles, it lasts for three days, it just makes my life so much easier – working, walking, being out with friends, it’s just always there. When I’m not on this, my sugars are always high. To me this is a godsend.”

Her insulin pump works in tandem with a continuous glucose monitor, which is even smaller, and also stays connected around the clock. She replaces the monitor every seven days. Both the glucose monitor and the insulin pod connect wirelessly to separate devices: one displays the blood sugar level, the other determines how much and when to dose the insulin, based in part on the information she inputs.
“If her blood sugar is high, it’s going to calculate how much insulin she needs to bring it down, and then she also puts in the grams of carbs that she’s eating, so that will calculate automatically how much to give her for the carbs as well as the high blood sugar,” Kostak says.
“All I have to do is push a button and it gives it to me,” Apanaovitch says.
Apanovitch is an example of a diabetic who accepts her disease and her responsibility to take the necessary steps necessary to manage it. Not everyone is a good fit for an insulin pump. Kostak says about a quarter of her patients use some version of the technology.
“If you don’t admit you have a life-threatening illness, you could die,” Apanovitch says. “And I don’t want to die, I don’t want to lose my legs or my fingers or my eyesight. So they say I have to go to the eye doctor every year, I go to the eye doctor every year. I take blood pressure medicine. And because all of my doctors are at UConn, they all connect.”
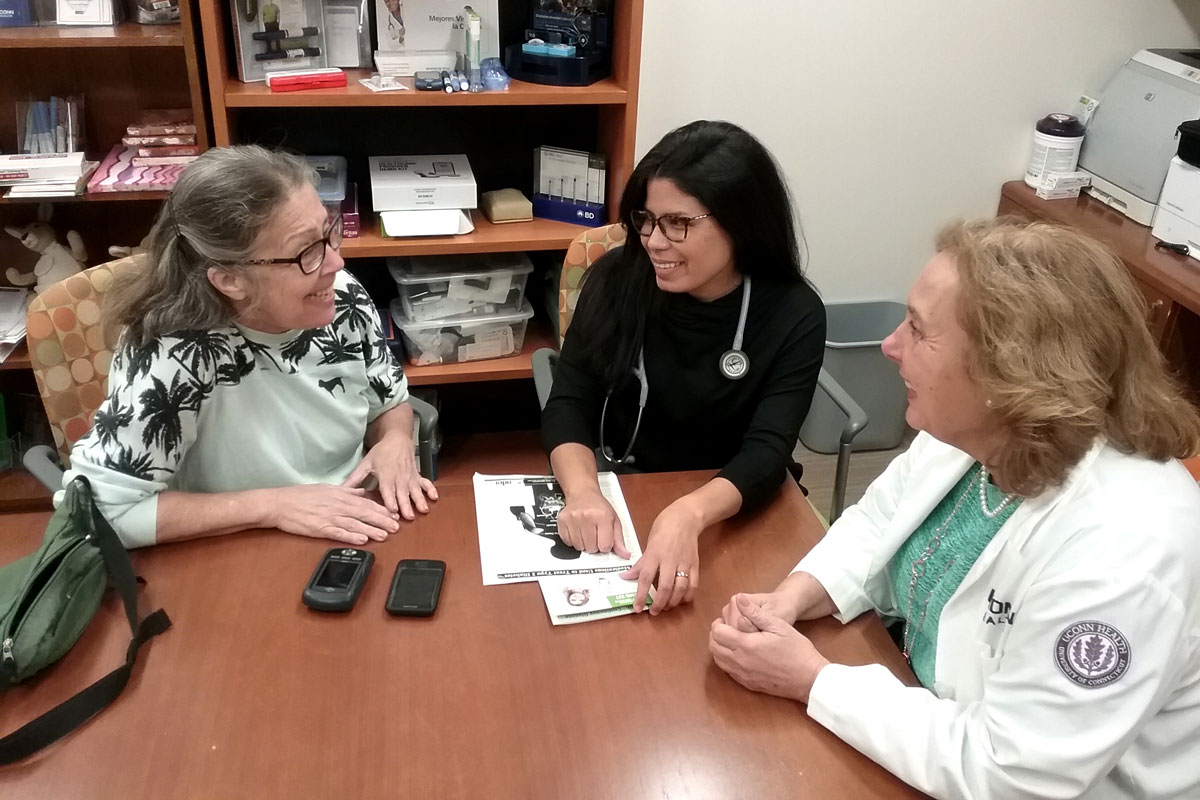
Part of that is embracing the advances in technology that help her keep her blood sugar levels within a healthy range. Another part of it is working with her health care providers, including Kostak, nurse practitioner Heather Myrick, Dr. Carl Malchoff, and nurse practitioner Luriza Glynn (and until her recent retirement, nurse educator Lori Fomenko).
“My diabetes team, I feel like they’re family,” Apanovitch says. “If I’m having a hard time and my sugar’s going up, they always talk me through it. If you can get a diabetes health team that makes you feel like, ‘You’re not a bother, we want to help you,’ – they’ve been absolutely fantastic. And the education, not only did they educate me, but some of my family members came in and they were educated, too. Education is very, very important, not just for the diabetic, but for the family members. But my diabetes team to me is family.”
Learn more about diabetes care at UConn Health, or call 860-679-2626 for a consultation.