During the COVID-19 pandemic, there has been a sharp decline nationwide in people seeking care for heart conditions and stroke in particular. These conditions do not get better on their own and emergency care should not be delayed. According to UConn Health’s stroke experts “Time is Brain”.
According to Dr. Mason Leeman-Markowski, a neurologist at UConn Health, the time interval from the onset of stroke symptoms to the time of treatment is one of the most important factors influencing stroke outcome. The brain does not start to die immediately after an artery is blocked. This process is more prolonged, and in favorable situation takes several hours. During these several hours everyone needs to act quickly and decisively. With every passing minute, there is additional and cumulative neuronal loss. The sooner a successful reperfusion therapy is implemented to restore proper blood flow to the brain, the smaller will be the final neurological deficit.
“If a patient or patient’s family notice symptoms reminiscent of a stroke, the best thing to do is to place a 911 call. I would discourage patients or family members from calling friends, other family members, waiting for an answer from their primary care physician, etc. A 911 call is the best thing to do,” says Leeman-Markowski.
Dave, a recent stroke patient at UConn John Dempsey Hospital, stresses that advice too. One Monday afternoon as he took a phone call at his home he became extremely dizzy. “It felt like the room was spinning,” he says. He fell to the ground and instructed the person on the phone to call 911.
Dave, 56, from Simsbury, had no known stroke risk factors. He is very active walking daily, playing hockey several times a week and racing sailboats. He’s generally a healthy individual and had no warning signs that anything was wrong.
EMS’ advanced notification from Dave’s home to the UConn John Dempsey Hospital’s Emergency Department where there is a dedicated Stroke Center activated the hospital’s swift stroke team’s response that whisked him from the ambulance directly to CT scan machine in the ED. That system works so that patients, like Dave, can rapidly receive TPA (a time-sensitive blood-thinning medication that helps reverse stroke) well below or within the “golden hour” care window.
“When we heard that a 56-year-old with stroke-like symptoms was coming in through our stroke alert system, our senses heightened,” says Jennifer Sposito, RN., MSN, stroke coordinator at the UConn Health Stroke Center.
After the age of 55, the risk of stroke doubles every decade. It is a reminder that strokes can affect younger adults, too. Over the last 10 years, there has been a 44% rise in the number of young adults (18 to 65) hospitalized for strokes.
“Most strokes occur in people 65 or older, but about 10% of strokes occur in people under 45 years old,” says Dr. Gracia Mui, co-director of UConn Health’s Stroke Program and Intensive Care Unit. “Often younger people do not recognize they are having a stroke because it’s usually seen in the older population.”
After several days in the hospital, Dave quickly recovered and was home where he started walking with his wife and dog again and was even mowing the lawn less than a week after his initial stroke.
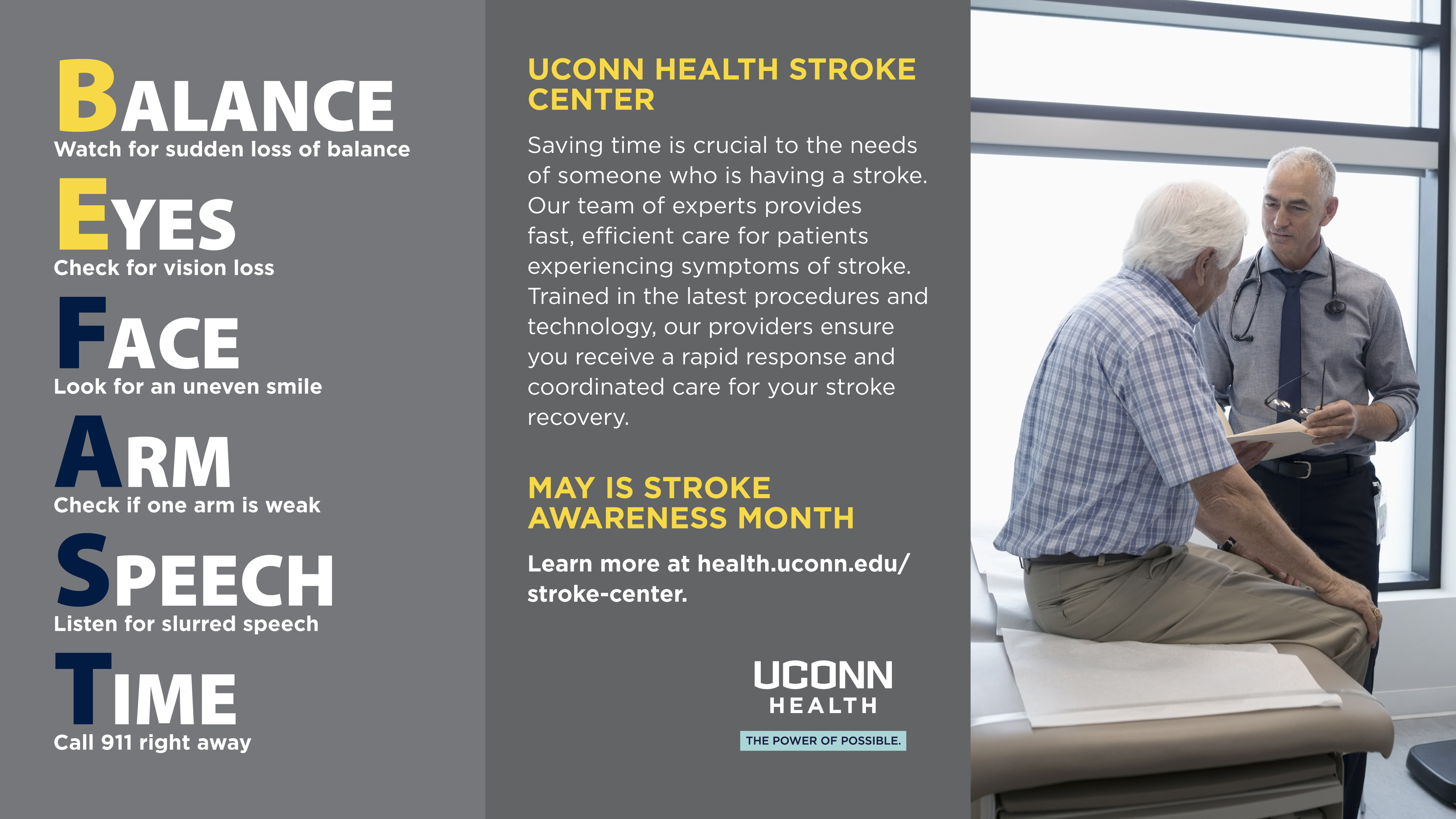
Know the Signs of a Stroke
It’s important to recognize the signs of stroke and to be sure that you or a loved one receives care quickly.
A simple way to remember the warning signs of stroke is BEFAST:
B – BALANCE: Watch for sudden loss of balance.
E – EYES: Check for vision loss.
F – FACE: Does one side of the face droop or is it numb? Ask the person to smile. Is the person’s smile uneven?
A – ARM: Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
S – SPEECH: Is speech slurred? Is the person unable to speak or hard to understand? Ask the person to repeat a simple sentence, like “The sky is blue.” Is the sentence repeated correctly?
T – TIME: If someone shows any of these symptoms, even if the symptoms go away, call 9-1-1 and get the person to the hospital immediately. Check the time so you’ll know when the first symptoms appeared.
Additional symptoms of stroke can include:
- Numbness or weakness of face arm and/or leg
- Acute vision changes
- Difficulty in speaking
- Trouble in understanding simple statements
- Confusion
- Trouble in walking or maintaining balance
- Sudden severe headache
Seek emergency care when you need it. UConn Health’s Emergency Department and its dedicated Stroke Center team are ready 24/7 to help you safely and promptly.