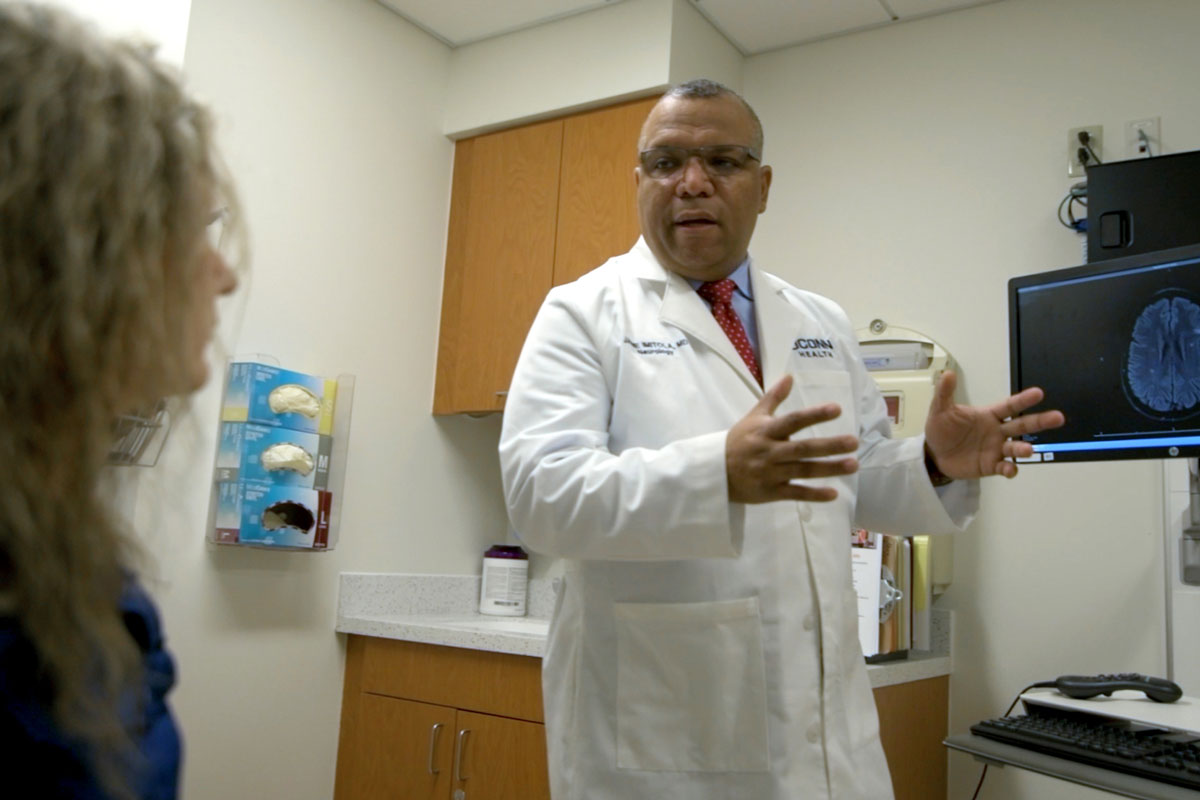
Amid the COVID-19 pandemic, there is a growing concern that patients taking immunosuppressive medications may have an increased risk for severe COVID-19. Dr. Jaime Imitola, director of UConn Health’s Division of Multiple Sclerosis and Translational Neuroimmunology, explains.
What has you worried about patients with multiple sclerosis or other conditions that require immunosuppressive therapies?
Due to exposure concerns, patients tend to follow strict shelter-in-place orders and remain at home even if they have symptoms. At the same time, these patients may have relapses of MS or worsening symptoms that may not be diagnosed or treated on time for fear from the patients to come to the hospital. Furthermore, patients with chronic MS are at risk of progression and need MS medications that are immunosuppressive, creating a challenging and uncertain situation for MS doctors and their patients that needs to be balanced with extreme care. More notably, the most challenging scenario is of a MS patient on immunosuppression who gets infected with COVID-19. That is why answers about COVID-19 in MS patients are critical to obtain to dispel misinformation and provide adequate long-term care, especially since the pandemic may not be over in the short term.
We encourage MS patients to call their doctor right away if they develop new neurological symptoms to find a suitable way to manage their care. At the same time, be safe about the CDC and local authorities’ recommendations.
Are MS patients at greater risk to contract COVID-19?
MS itself does not increase the risk of infection. However, those who are taking medications that suppress the immune system are at risk of having a harder time once they are infected. For anyone, any fever or viral infection, such as the seasonal flu, can exacerbate MS symptoms. And COVID-19 can lead to more severe symptoms in those who already have a significant neurologic disability. But there’s no indication that COVID-19 increases the chance of an MS relapse or worsening the disease. We have a full set of guidelines for COVID-19 and MS front and center on our Multiple Sclerosis Center home page. While the data available so far are not showing evidence of COVID-19 ravaging the MS population, it understandably is causing a lot of fear.
What should MS patients do if they believe they may have contracted COVID-19?
Patients need to understand, if they notice a change in their disease or their disease progressing, or if they have an MS relapse, they need to call their doctor right away. There’s a careful balance of the risk of COVID-19 and the worsening of their disease.
Those who develop symptoms like high fever, respiratory problems, deep dry cough, or fatigue, it’s best to call your primary care doctor first. Of course, if acute respiratory issues develop, go to the ED but call ahead if possible. Absent severe symptoms, the recommendation likely will be to stay home. Try to separate sick people from well people in the home as much as possible.
Also, patients may have a relapse or they may present with initial symptoms of MS. Therefore, they need to be seen in the ED and quickly diagnosed and promptly treat their relapses as well as any other medical urgency from strokes to heart attacks during this pandemic.
Describe the role of telemedicine in treating/managing MS?
Telehealth is helping a great deal and probably will change neurology care moving forward for those patients that are stable and may need less in-person follow-up and in cases where the patients are confined at home because of lack of mobility and in case of the pandemic. We want to limit the mobilization of the patients to decrease risks.
What about when things start getting back some kind of normal?
Many clinics have been closed, and when things start opening up again, there’ll be a backlog of patients who might need help. Plus, it may take a while for people to be comfortable with the idea that the hospitals are ready for people who don’t have COVID-19. But patients need to understand, if they notice a change in their disease or their disease progressing, or if they have an MS relapse, they need to call their doctor right away. There’s a careful balance of the risk of COVID-19 and the worsening of their disease. We understand more and more the way that the virus transmits and what precautions to take in the clinic.
When it’s finally time to start getting back to some kind of normal, what precautions do people with MS need to take?
I think that “normal’ will take a long time. There will be a gradual transition, and when we do open up again – and by that I mean when we start lifting the recommendation that everyone stay home as much as possible – it still will be a gradual process that requires great care and discretion. It is understandable for people with MS to ask ‘Are we okay to go back?’
Patients will be required to answer questions related to exposure, recent travel history, fever, cough, shortness of breath, or recent exposure to anyone with those symptoms or to patients who’ve been diagnosed with COVID-19.