While the COVID-19 pandemic is often described as unprecedented, there is a recent viral epidemic that researchers in UConn’s Institute for Collaboration on Health, Intervention and Policy (InCHIP) say can offer lessons about social and behavioral responses to disease.
In a special commentary published recently in the Journal of Behavioral Medicine, Lisa A. Eaton, associate professor of Human Development and Family Sciences, and Seth C. Kalichman, professor of Psychological Sciences, address multiple levels of disease intervention that began 40 years ago during the HIV/AIDS epidemic.
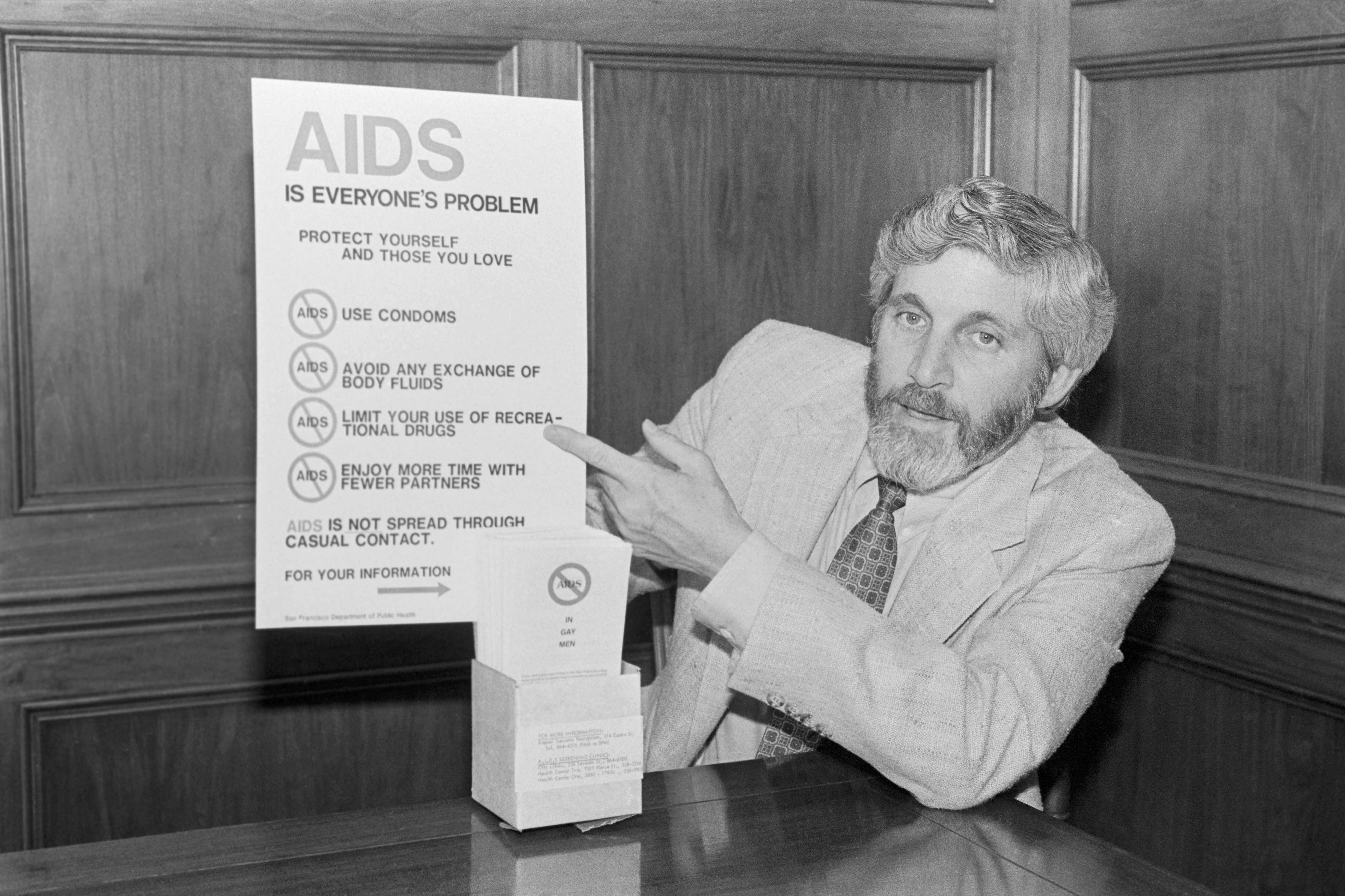
Human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) were initially identified in 1981 as rare cancers among gay men, Haitian immigrants, intravenous drug users, and hemophiliacs. Twenty years later, the introduction of protease inhibitors and other antiretroviral medications provided treatment for the disease that has caused about 32 million deaths worldwide.
“Social and behavioral scientists aiming to contribute to the containment and mitigation of COVID-19 will be well-served by the lessons we have learned in HIV prevention and research,” the researchers say. “The lessons we have learned should be evaluated for use in the case of COVID-19 and for future pandemics.”
The researchers say the Social Ecological Model of Health, which was developed to understand how personal and environmental factors are inter-related, helped public health officials learn lessons to guide the prevention and treatment of HIV/AIDS. The idea was the focus of the Russian-American psychologist Urie Bronfenbrenner, who studied the effect of environmental and social influences on child development and led to the creation of the Head Start program in 1965.
Eaton says that until there is a vaccine or a curative treatment, the primary option to halt the spread of COVID-19 depends on social/behavioral action, noting the efforts by health experts and public officials to promote such messages.
There are four key areas that serve as a reference point for understanding and elaborating on social and behavioral lessons that resulted from research in HIV prevention and treatment: intrapersonal factors, interpersonal factors, community influences, and societal activities.
Eaton says changing individual behavior is difficult to achieve, and that multiple approaches to supporting change are imperative.
“At this point, we’re mainly reliant on social and behavioral responses to slow COVID,” she says. “Some of the most important things that we’ve learned in terms of how people respond to prevention is that sustained behavioral change is very challenging. One of the examples I use that most people can relate to is achieving and maintaining a healthy weight, which is exceedingly difficult for most adults. People are very attuned to rationalizing their choices, both good and bad, when it comes to health. We are willing to accept a certain level of risk that comes with the benefits of living. Preventing COVID is not an exception: people will rationalize why they believe that some level of risk is acceptable.”
At the same time, interventions by government and health experts are undermined by mistrust of medical experts and erroneous conspiracy beliefs, just as they were during the initial reports about HIV/AIDS, the researchers say, and such mistrust and doubt is based on a history of the abuse of vulnerable populations who have difficulty receiving care.
“The historical impact of racism cannot be understated, and has led to large inequities in health care infrastructure and access,” Eaton says. “Although some media reports have made it appear that COVID related health disparities are a novel observation, these disparities exist and have existed across all diseases and health outcomes. It’s no secret that people with the most socio-economic disadvantage are also going to face the greatest barriers to accessing appropriate medical facilities and care providers. Individuals showing up late in disease stage to the hospital, not showing up at all, or having greater challenges to adhering to a treatment plan are outcomes that are part of the broader context of health care inequity that we have observed over the history of medicine.”
Multi-level interventions in the community at large are essential in stopping the spread of disease, the researchers note, and have the potential for high efficacy in altering the course of the disease, but must be maintained even as people become anxious to relax their behaviors.
“Having seen some of the same behaviors and cognitions unfold in HIV prevention, one of the things that I’m concerned with is fatigue and we’re observing it already. There are some people who won’t participate in social distancing,” Eaton says. “We’re seeing groups aligned in protest. People start to rationalize why it’s okay to spend time with other people. For myself, I’m aware of these things and I still find myself rationalizing. That is the fatigue that we absolutely observed in HIV prevention. People will prioritize immediate gratification as opposed to delayed long-term gain. It is critical to get ahead of fatigue with setting the appropriate cultural tone for supporting long-term gain. A lack of alignment in leadership contributes to the fracturing that we’re currently experiencing on the ground level.”
Engaging multiple sectors in society to address health or environmental issues is a cornerstone for community or social mobilization, the researchers say.
“Particularly in the earliest days of the HIV epidemic in the U.S., community mobilization was ultimately highly effective at challenging and changing the response to HIV at the federal level,” Eaton says. “But efforts were sustained and hard-fought. We are observing similar patterns with COVID-19 where communities most affected (e.g. high population density cities and communities initially impacted) are appealing to the broader community for a national level response.
“Likewise, we recognized that total risk elimination was not possible, and what we refer to as harm reduction sort of became the law of the land for HIV. Which is likely the course for COVID. Harm reduction requires people to be thoughtful about reducing risk. It requires not living at either ends of the pole; there is no total risk elimination or total chaos, what remains is thoughtful decision-making.”