“At what point do knowledge and questioning become pessimism?”
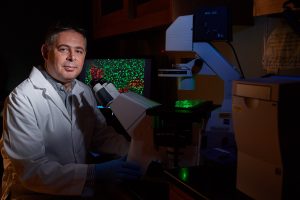
This was a question that came up in a recent conversation with UConn vaccine researcher Paulo Verardi. We met via Zoom to talk about the likely longer-than-desired road ahead for a vaccine for COVID-19.
Verardi cautions that in a time when hopes are high, the public needs to be informed and to have realistic expectations. This can be accomplished by digging into the history and science of vaccines, to understand past successes and failures in their development.
The conversation was sobering and one where we both had to stop and reflect on how surreal the current situation of the world is. We had spoken earlier in the year when the COVID-19 pandemic was just starting to gain notice, and never thought our next conversation would be virtual, after months in isolation.
Verardi is one of the researchers and lecturers for UConn’s massively popular COVID-19 course, and a collaborator in research aimed at finding a COVID-19 vaccine. In the online course, he lectures about vaccine development, frequently updating information to keep up with developments. One element is becoming more pertinent – vaccine research is full of pitfalls, like, for example, vaccine-enhanced disease (VED). A common respiratory infection called Respiratory Syncytial Virus, or RSV, can be deadly for the youngest members of the population. A vaccine for the disease was developed and administered in the 1960s. Unfortunately for some of those vaccinated children, the disease was worse, even leading to death. Similar “disease enhancement” has been noted for some vaccine strategies in animal studies for some coronaviruses like SARS-CoV.
“It is important to recognize that you cannot just develop a vaccine overnight, it takes five to twenty years, typically a decade or so, from the time you start developing a vaccine to the time that you may obtain FDA approval,” says Verardi. “It is a really, really long and expensive process because you have all of these checkpoints, to ensure safety and efficacy.”
The process requires development, supplies, animal testing, and human clinical trials – all of which are impacted by the pandemic.
For instance, vaccines typically require non-human primate testing during their development, and in the case of COVID-19, in high biosafety level facilities. Right now, even getting enough animals for testing is difficult, and there are only a limited number of those types of research facilities in the country, says Verardi.
Besides speeding the process along, Verardi brings up the point that currently in the United States all of our hopes are in a handful of companies – currently five — with three vaccines already in human clinical trials, and no further federal funding at the moment.
The three vaccines in clinical trials use the same nucleic acid strategy. Nucleic acid-based vaccines are experimental, and there are no approved vaccines in the US that use this strategy.
“If all of the focus in the US is on these nucleic acid-based vaccines and they do not work, essentially we have no plan B right now,” says Verardi.
“This is a significant concern because despite many years of research on other human coronaviruses such as SARS‑CoV and MERS‑CoV, no vaccines of any kind have been approved. Another major concern is that some experimental vaccine studies in animal models suggest that insufficient protective immunity against coronaviruses such as SARS‑CoV may induce enhanced susceptibility to respiratory disease. In other words, inadequate or weak vaccines may not only lead to poor protection but also to vaccine-enhanced disease in COVID‑19 patients.”
Rather than put all of our hopes on a handful of vaccines using the same strategy, we need to pursue every approach available says Verardi, and to look at qualities that have made other vaccines successful. Smallpox is the only disease declared eradicated to date, and Verardi says we can apply lessons from this achievement to succeed in finding a COVID-19 vaccine.
Verardi points out that different vaccines confer immunity differently and to different degrees. In the case of smallpox and measles, immunity is typically for life. With other vaccines such as tetanus, diphtheria, and pertussis, immunity may wane, requiring booster immunizations.
The need for multiple approaches and vaccines for a single pathogen is well-illustrated in the story of polio. There are pros and cons with every vaccine.
The Sabin oral polio vaccine is a live attenuated vaccine. Pros: It is an oral vaccine and once administered, the virus replicates and elicits a strong immune response. This means the vaccine can be given at a low dose and it also makes the vaccine more cost effective. An added bonus and less known fact is that the attenuated vaccine virus is shed and can potentially spread to other people, thus amplifying the vaccination effort, particularly in impoverished communities. Cons: In a small percentage of patients, the virus can revert back to a pathogenic form, and cause disease. The vaccine is also not stable at room temperature (requires a cold chain), which can hamper vaccination efforts in developing areas.
The Salk polio vaccine is a killed vaccine. Pros: There is no risk for reversion of the virus and disease. Cons: It is an injection given in a spaced-out series of shots, making it more difficult to fully vaccinate everyone. It is also considerably more expensive to produce.
In the US, the Salk polio vaccine is given to children. In the remaining few areas around the world where polio is endemic and eradication efforts are underway, the oral polio vaccination is given due to its efficacy, low cost, and ease of administration. However, due to the live attenuated vaccines ability to revert back to its pathogenic form, there is a real need to give the Salk killed vaccine to achieve full eradication of the disease.
“We need a ‘one shot and you are protected’ kind of vaccine for COVID-19,” Verardi says. “We do not have much experience with coronaviruses in humans because human coronaviruses are typically common-cold viruses. No one has really worked with them before because they are relatively mild, at least until SARS came onto the scene in 2003. Much of what we know about coronaviruses is from the veterinary field and the lessons learned tell us this is going to be a difficult trip, not a walk in the park, as we don’t have good vaccines for coronaviruses. For instance, when considering live attenuated vaccines for an avian coronavirus that causes respiratory disease in chickens (Infectious Bronchitis Virus or IBV), if you attenuate the vaccine virus too much you do not get good, lasting protection. If you do not attenuate it enough, you can get disease from the vaccine.”
Besides striking the right balance for immunity, another important detail needs to be considered – logistics. A vaccine may not be feasible for every situation. For instance, in some areas of the world where technologies like refrigeration are at a premium, having a vaccine that does not need to be kept cold can help ensure everyone has access. An excellent example of this is again seen with the smallpox vaccine, which didn’t need to be refrigerated.
When a reliable vaccine is developed, the next hurdle is to produce 7.8 billion doses (assuming the vaccine can be administered as a single dose). It is a tall order to produce even 330 million for the population of the US, says Verardi.
We need to find the balance, we can’t have the world’s economy in the state that it is in, and we are in a desperate situation. Desperate situations call for desperate measures. — Paulo Verardi
For smallpox, Verardi says this problem was overcome by the ease in how the vaccine was made: the first-generation vaccine developed in the 20th century did not differ much from the original vaccine developed centuries ago.
The formulation requires a shaved calf (where ‘vacca’, in vaccination comes from, it is Latin for ‘cow’) and a dose of ‘seed’ virus such as the cowpox virus (and in modern times vaccinia virus). By using the closely related vaccinia virus, the vaccine protected against smallpox. Once the virus was applied to the skin by scarification, the calf developed vesicular lesions and after about a week or so Verardi says the next step was to harvest them by scraping. This material was then ground and resuspended in buffer and used as the smallpox vaccine. Several hundred thousand vaccine doses were produced per calf.
This vaccine was made by multiple countries around the world, is effective, low cost, and low tech. It was simple and inexpensive to produce the vaccine, and even developing countries could produce their own vaccine doses – another important element in the disease eradication effort. This do-it-yourself mass production may not be possible with some modern vaccine approaches.
With all of this in mind, Verardi says we need a collective and coordinated effort like that seen for smallpox for developing, producing, and deploying vaccines against COVID-19,
“In the US we are all just hoping that these experimental vaccine approaches will work and unfortunately vaccine development doesn’t work that way. We need to think ‘outside the box.’”
We are living in a profoundly uncertain time. For most of us, our lives have been put on hold as the world waits for solutions to the pandemic. From hopes that seasonal changes will halt the virus, to controversial drugs, to putting all of our eggs into a couple of baskets in the race for a vaccine. What is clear is that pausing our lives is slowing the spread, but life must go on. However, getting back to “normal” may not happen until we have a vaccine. Verardi says it is important to recognize the world cannot remain on hold until then.
“We need to find the balance, we can’t have the world’s economy in the state that it is in, and we are in a desperate situation. Desperate situations call for desperate measures.”
To keep up with the latest COVID-19 research happening at UConn, visit the COVID-19 Research and Grants web page.
The COVID-19 Alumni course will launch next week on Monday June 22nd. Alumni can enroll through Blackboard Genius. Potential learners can search for a course register for it all from one page. Alumni will be sent an email with a link to the course on HuskyCT. Anyone who is not a UConn alumni that has interest in the course can email Ruth Kustoff at Ruth.kustoff@uconn.edu



