It’s very easy to take our ability to swallow for granted. That is, until our food is slow to go down, or doesn’t go down at all. For many of us, this will happen rarely if at all, but when it does, it can be much more than a nuisance; it can be life-threatening.
Over the last several months UConn Health has built a specialty practice dedicated to diagnosing and treating problems with the esophagus. Led by Dr. Houman Rezaizadeh in the Division of Gastroenterology and Hepatology, the UConn Health Esophageal Disease Center is an alliance of specialists equipped to focus on problems with the gateway to our digestive system.
“We have comprehensive diagnostic options in terms of being able to offer nearly every modality to diagnose these disorders,” Rezaizadeh says. “And then we have a full team of specialists committed to and interested in these disorders. It’s hard to find somewhere where they have a team of surgeons, a thoracic surgeon, a GI oncologist, a pathologist, and a radiologist specifically interested in this, all along with a taste and swallow center.”

Access to all this expertise in one place can fast-track care for patients.
“If there’s somebody with constant throat clearing, throat burning, or changes in voice, I might say, before seeing me, go see ENT first, because they can do a laryngoscopy to help expedite their care and save them time,” Rezaizadeh says. “Then if ENT thinks they need to also see me, then they’ll refer to me and we try to get them in as soon as possible for evaluation.”
Rezaizadeh has been with UConn Health for eight years. He joined the faculty in 2015 after completing UConn’s Gastroenterology-Hepatology Fellowship. He is uniquely trained in radiofrequency ablation and endoscopic mucosal resection (EMR), two specialized procedures to remove lesions or potentially cancerous tissue from the esophageal wall.
“Part of my passion is doing preventive medicine with screening patients with reflux for Barrett’s esophagus, which is a precursor to cancer,” he says. “We try to catch them in early stages so that we can prevent progression, and maybe ablate them as needed. That’s a major issue right now. Esophageal cancer is dramatically rising in incidence.”
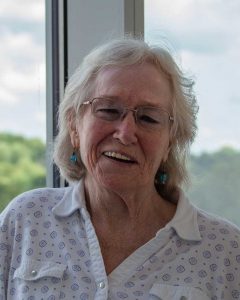
Mary Ellen Ferreria is a testament to that vigilance. About two years ago she started having trouble swallowing. A series of endoscopies would follow over the next several months, to dilate the gullet and try to find the cause of the recurring problem. But her food regularly would get stuck and she’d have to induce vomiting. GI providers elsewhere told her they couldn’t find the cause of the problem.
“I went through this for like a year, and the only thing I could get down was milkshakes,” Ferreria says. “Dr. R. kept insisting that there was something there with his biopsies. Luckily I had him. I still say he saved my life.”
He sent her to Dr. Stefan Kachala, a thoracic surgeon affiliated with UConn Health’s Esophageal Disease Center, for a robotics-guided procedure. That’s when the cancer was discovered.
“Lucky for me it was stage one, and he got it all out robotically,” Ferreira says.
That was in early 2019. After three months on a feeding tube, Ferreira gradually started making her way back to eating regularly. Subsequent endoscopies and CT scans have shown no signs of cancer.
Ferreira, 66, says she’s now able to eat just about anything, “as long as it’s small bites and small meals.”
Ferreria’s esophageal cancer was preceded by a diagnosis of Barrett’s esophagus. That was preceded by three decades of reflux, with regular consumption of antacids and heartburn medication.
“It’s not uncommon for people to just take over-the-counter antacids, and they don’t realize that they’re at risk for Barrett’s esophagus,” Rezaizadeh says. “It kind of becomes a backburner issue. They’re not realizing that the antacid is not going to treat their Barrett’s, that they need to be monitored endoscopically.”
One of Rezaizadeh’s objectives is to raise awareness that trouble swallowing is not a normal problem to have.
“There are people who have had some intermittent trouble swallowing here and there, and they don’t really pay close attention to it until they hit a tipping point where they can’t even eat,” he says. “We’re trying to catch those types of patients earlier to establish a diagnosis and begin treatment.”
Esophageal disorders range from frequent throat clearing to non-cardiac chest pain to cancer. Reflux and dysphagia, or difficulty swallowing, are among the more common.
Another condition, eosinophilic esophagitis, or EoE, is the focus of a new clinical trial for which UConn Health has applied to be a test site. There are no Food and Drug Administration-approved treatments for EoE and there are relatively few active studies of it.
“The therapy and management for esophageal diseases such as reflux, motility disorders, Barrett’s, eosinophilic esophagitis and even esophageal cancer screening have evolved significantly in the past decade,” says Dr. John Birk, chief of UConn Health’s Division of Gastroenterology and Hepatology. “Having a focused program dedicated to treating these conditions will provide for better patient care.”
Learn more about the UConn Health Esophageal Disease Center. Medical assistant Stephanie McGinn coordinates the care among all the specialties that make up this group. Her number is 860-679-3040.



