So many common ills in our society are caused not by microorganisms but by social constriction — poor education, poor housing, poor food. Even when a virus is the primary cause of illness, social conditions can exacerbate the disease. The Covid-19 pandemic shined a bright light on the unhappy truth that structural inequities limit access to health care in America. Doctors who are unaware of these systemic barriers to health cannot truly help their patients who face them, and doctors who are aware of them can feel powerless to do something about it.
But they aren’t.
The students at UConn Health’s schools of medicine and dentistry know that. Beginning with the 2021 graduating class, every medical student at UConn Health must complete a capstone project in public health before graduating with their MD.
Health disparities and health equity “are a fundamental thread that runs throughout the curriculum from the first days and weeks that students arrive until they graduate,” says Zita Lazzarini, director of the Division of Public Health Law and Bioethics in the Department of Public Health Sciences at UConn Health and an associate professor in the School of Medicine.
UConn Health’s School of Medicine was the first in the nation to require students to complete a certificate curriculum in social determinants of health, and the program is being emulated by other medical schools, according to School of Medicine dean Dr. Bruce Liang. Students in the UConn School of Dental Medicine have the option to complete the certificate.
“Health disparities among racial and ethnic minorities and between the most affluent and least well-off remain unacceptably high in the U.S. We want our graduates to be fully equipped to recognize and reduce health disparities in their communities through direct patient care, research, and advocacy,” Lazzarini says.
Jump (For Your Health)
“Growing up, I was aware of disparities,” says Srinath Ramanan, who immigrated to West Haven, Connecticut, from India with his family at age 6. His own family never suffered from food insecurity, but Ramanan wasn’t oblivious to the struggles of others in his diverse apartment building. And now, the second-year medical student is doing something about it, helping families get fresh food and educating kids about sugar and health.

“I want to get as many people involved as possible! The magnitude of the effect will be greater,” Ramanan says of the next UConn Just Us Moving Program (JUMP) event, which is scheduled for the week after we talk. JUMP’s mission is to get people moving more and eating more healthy food.
The program, which is sponsored by the Aetna Foundation and run by the Connecticut Convergence Institute for Translation in Regenerative Engineering at UConn Health, is situated in the Urban League of Greater Hartford and provides the tools to avoid or control diabetes, a big problem in the neighborhoods of North Hartford that lack grocery stores. Ramanan will be manning the sugar table, a display and short presentation he designed along with fellow student Vishruthi Palanivel. They use piles of sugar packets to illustrate to kids just how much sugar you should consume in a day versus how much sugar is in common convenience foods. (Spoiler: a single Gatorade’s mountain of sugar dwarfs the daily limit.)
Ramanan learned of JUMP through through associate professor Zhao Helen Wu during his first year. He and a buddy from engineering school in undergrad had already started working on health disparity issues, and JUMP’s mission fit right in. He began working on the presentations, and then this summer he started work on aeroponic food towers in the Urban League’s building in the Asylum Hill neighborhood. The food towers can grow greens, herbs, and small vegetables year-round using water, nutrients, and light provided by the Urban League. Essentially, it’s an indoor community garden — the plan is to have each one adopted by a local family, who can plant what they want and harvest whenever they like, just by visiting the Urban League location where their food tower lives.
For Ramanan, empowering people with the knowledge to make good choices is a key piece of addressing disparities. “If we have education, we have more control over what we do,” he says.
Getting to the Root
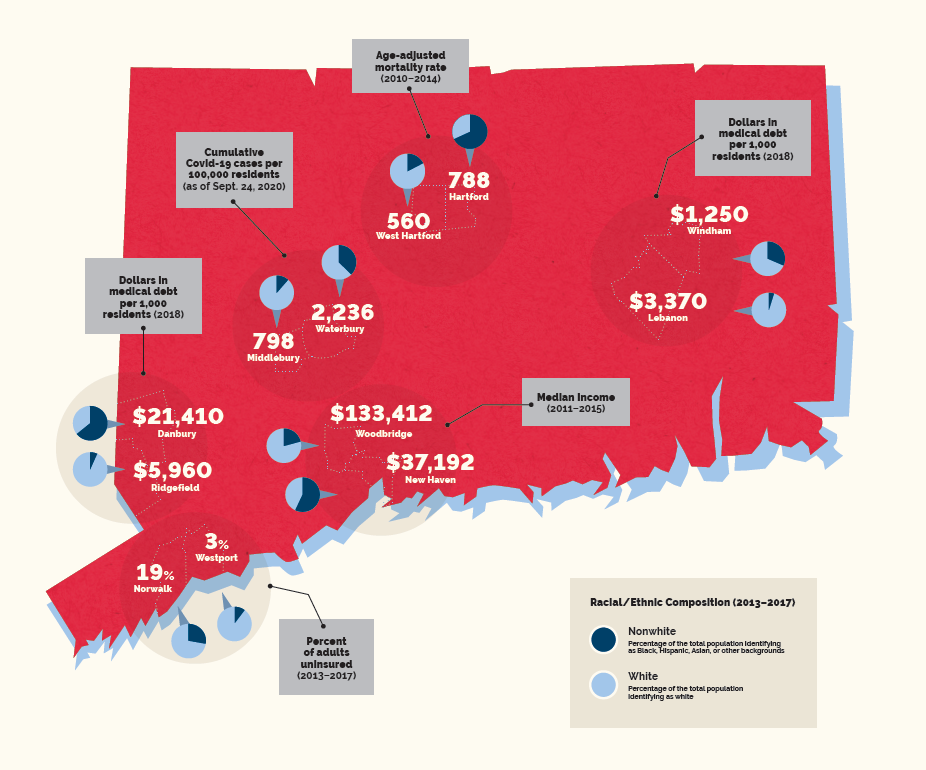
The north side of Hartford where Ramanan tends the food towers is only a 10-minute drive east of UConn Health’s Farmington campus, but a person’s life expectancy at birth drops a year for every minute you travel. That is to say, someone born in West Hartford or Farmington can expect to live 86 years. Someone born in North Hartford, on average, won’t live past 75. The disparities between these two areas echo disparities in the U.S. as a whole.
Teaching about their effects on people’s health, and how physicians can help, is an integral part of the curriculum in the medical and dental schools.
In 2015, North Hartford, which includes the Northeast, Upper Albany, and Clay Arsenal neighborhoods, was designated a federal “Promise Zone” under an Obama-era program that partnered with neighborhoods around the country to combat staggering rates of poverty, unemployment, food insecurity, and violent crime.
During the health equity module in the students’ first year, hospitalist Dr. Kirsten Ek takes the students on a tour of the North End neighborhood. They visit the Parker Memorial Community Center and a local church, chat with kids and community leaders, survey local parks and housing, and try to figure out where the pharmacy is, and the grocery store (there isn’t one).
“If you’re going to practice in Hartford, why not know it?” says Ek, an assistant professor of medicine who directs the course “Patient Advocacy in Communities, Teams & Health Systems.”
There is actually one grocery store on the edge of the area, but it’s not accessible via public transit and it’s not well stocked. Ek says she bought oranges there one day for the students and cleaned out the whole supply.
Two days later she stopped in again, and they still hadn’t restocked oranges.
“We want the students to see how structural inequities lead to health effects,” Ek says.
Many of the students’ public health capstone projects are inspired by their visit to the neighborhood. Some of these projects, like Ramanan’s, involve direct activism in the community. Others take place more behind the scenes.

For instance, third-year medical student Jessica Bertenshaw is focusing on electronic health records. Doctors use them as electronic files to organize patients’ information. Everything that relates to a patient’s health has a place in the record. Electronic health records even have special codes, called Z codes, that indicate social factors such as food insecurity or unsuitable housing. The problem is that most doctors don’t use them.
“Studies show that if Z codes are actually coded into the record, people are more likely to get referred to services. You can get more to the root of their health problem” if you address the social limits they’re facing, Bertenshaw says. UConn Health, for example, has social workers on staff who can connect patients with food, transportation, or other resources they might need. But if the doctor interviewing the patient merely
notes the need in the written record, it can get buried. Z codes make it easy for that need to get seen and addressed.

To raise awareness of Z codes, Bertenshaw plans on working locally, meeting with resident doctors as they rotate through St. Francis and Hartford hospitals to remind them of the codes and urge them to act on them. She also plans to analyze whether the residents who received extra training on Z codes use them more.
Other student projects focus on more concrete aspects of physician education. Fourth-year student Savannah Alvarado has been working with UConn Health dermatologist Dr. Hao Feng to get better visual imagery of skin diseases on darker-complexioned people, for example.
“It is no secret that pathology appears very different on dark skin and that trainees do not have much exposure to training on dark skin, for a long list of reasons. Unlike the lungs, liver, or kidneys, which look roughly the same regardless of race or ethnicity, the skin and hair obviously don’t, so there is a huge need for specific training in this area,” Alvarado says.
Alvarado and Feng are currently working on a paper that provides a clinical guide for photography of dark skin.
Sometimes a student brings her passion for a particular community into her project. Jessica Weeks had worked with youth in juvenile detention when she was an undergraduate. When she came to UConn Health, she decided to start a similar program here. It wasn’t easy — there was no relationship between the institutions, and it took a lot of phone calls, emails, and persistence — but eventually she got a weekly program up and running called Better Futures. Every Wednesday night, a group of medical and dental students went to a Connecticut juvenile detention center to mentor the boys and young men, some as young as 12, in life skills they’d need when they got out. How to write resumes and interview for a job. How to get a driver’s license. Coping strategies like meditation.

“A lot of these children come from the worst of the worst situations,” says Weeks. Some of them still cannot read easily and lack other basic skills. Despite the neglect they’ve suffered up to this point, Weeks believes that most of these boys can improve their lives. They just need the resources. She plans on becoming a child psychiatrist and continuing to work with incarcerated youth throughout her career.
“I will always fight for their rights and continue to work on behalf of these young men,” Weeks says. As a fourth-year medical student, she’s currently working to make sure the mentoring program continues after she graduates.
A Salutary School
Before we go on, we should note the elephant in the room. Most of the student projects we’ve mentioned that take place in North Hartford work primarily with people of color. That’s because most of the residents of North Hartford are people of color, and the area in which they live puts them at significant structural disadvantage. But as Dr. Kenneth Alleyne, an orthopedic surgeon and a member of the UConn Health Board of Directors, likes to point out, we have to resist the temptation to racialize health.
Residents of North Hartford are more at risk of diabetes not because they are Black or Latino but because they don’t have easy access to decent food in their neighborhood. If they lived in a poor section of Appalachia they would more likely to be white and suffer from the same troubles. Constant stress due to the tenuousness of a low income and its accompanying worries takes a physical and mental toll, depressing people’s resilience and immune systems. This is one of the many reasons why pregnancy, cancer, and now Covid-19 all take a higher toll on people of color who live in disadvantaged neighborhoods in our state.
Although many of these things are out of doctors’ control, physicians often have access to resources that can help people change their structural determinants of health for the better.
“Disparity is pervasive, and it needs to be eliminated,” says Liang. As dean of the medical school, he is acutely aware that having a diverse student body — UConn Health ranks among the top 10 medical schools in the nation for diversity — is not enough. Neither is simply describing UConn Health’s commitment to health equity in a public statement. The institution is taking action.
The first action is in the education of the students. In addition to the health equity module, students are required to take four courses in public health, with a focus on epidemiology, biostatistics, and health disparities. The medical and dental schools have also started training students in cultural competency, recognizing that people from different backgrounds may express symptoms and pain differently. The capstone project in public health is the culmination of this coursework.
In addition to raising students’ awareness of these issues and training them to respond, the capstone project and community efforts in different underserved areas also serve to give students a more personal connection to the communities they serve. The more of a connection the students have with the area, the more likely they are to return and practice there in the future.
UConn Health has also begun implicit-bias training for students, faculty, and clinical staff. This training tries to help people recognize unconscious bias they might have against certain groups of people. The hope is that they will self-correct to prevent bias from coloring their treatment decisions.
Eliminating bias and disparities “requires a cultural change, reflection, awareness, and self- monitoring. And everyone has to be rowing in the same direction,” Liang says.
This story appeared in the UConn Health Journal fall 2020 issue.