Some of the brightest minds in dermatology and surgery are in agreement on the first clinical practice guidelines for reconstructive procedures following skin cancer resection.
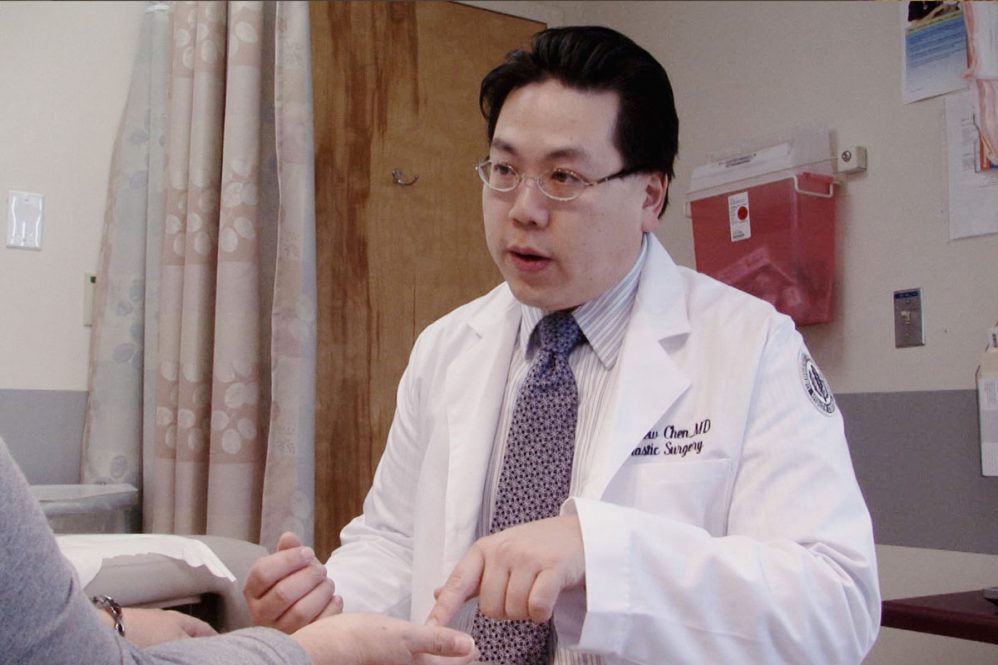
Dr. Andrew Chen, UConn Health’s chief of plastic surgery, is the lead author of the guidelines, published concurrently in Plastic and Reconstructive Surgery, a journal of the American Society of Plastic Surgeons, Dermatologic Surgery, and the Journal of the American Academy of Dermatology.
Chen was chosen to lead a group of stakeholders including dermatologists, plastic and reconstructive surgeons, dermatologic and Mohs surgeons, head and neck, and ear, nose and throat surgeons, and others, including patient representatives, to analyze the evidence and make recommendations to guide physicians as they care for patients who need reconstructive surgery after having cancerous skin removed.
“We studied the evidence to make determinations on antibiotics, what are the recommendations with respect to pain control, the use of anticoagulants, as well as the timing of reconstruction,” Chen says. “What are the best practices? What kind of things should we be doing or should we not be doing?”
The work group’s recommendations include:
- Reconstructive surgery does not have to be done immediately following skin cancer resection in all cases.
- Clinicians should not routinely prescribe systemic antibiotic therapy in the time between resection and reconstruction.
- Systemic antibiotic therapy within 24 hours of reconstruction may be recommended when the surgery is done in a hospital or facility setting, but not when it’s done in an office-based setting.
- Blood thinning or anticlotting agents should continue for patients undergoing skin cancer reconstruction in an office-based setting, but in a facility setting, clinicians should coordinate with the physician who is managing those medications before the procedure.
- For pain management following skin cancer reconstruction, the first-line therapy should be acetaminophen and nonsteroidal anti-inflammatory drugs; routine prescription of narcotics is not recommended.
- Clinicians should discuss pain management, antibiotics, and anticlotting agents with reconstruction candidates.
- Clinicians may offer postoperative follow-up assessments.
“These guidelines are also going to lead to clinical performance measures,” Chen says. “That’s another thing we’re working on with the federal government, for the Centers for Medicare and Medicaid Services, which may guide how physicians are going to get reimbursed, rated, and assessed.”
Because there previously were no such guidelines, these recommendations are somewhat general in nature and represent a starting point. Additional research will be needed to come up with more specific and detailed recommendations in the future, Chen says.