Dr. Riqiang Yan, professor and chair of the Department of Neuroscience, has published a paper putting forth a novel combination of compounds that could dramatically improve treatments for Alzheimer’s Disease.
This paper was published in Molecular Psychiatry, a Nature journal.
Led by postdoctoral fellow Brati Das, the team discovered that combining positive allosteric modulators (PAMs) of metabotrophic glutamate receptor-1(mGluR1) with commercially available BACE-1 inhibitors can override the negative side effects of these inhibitors.
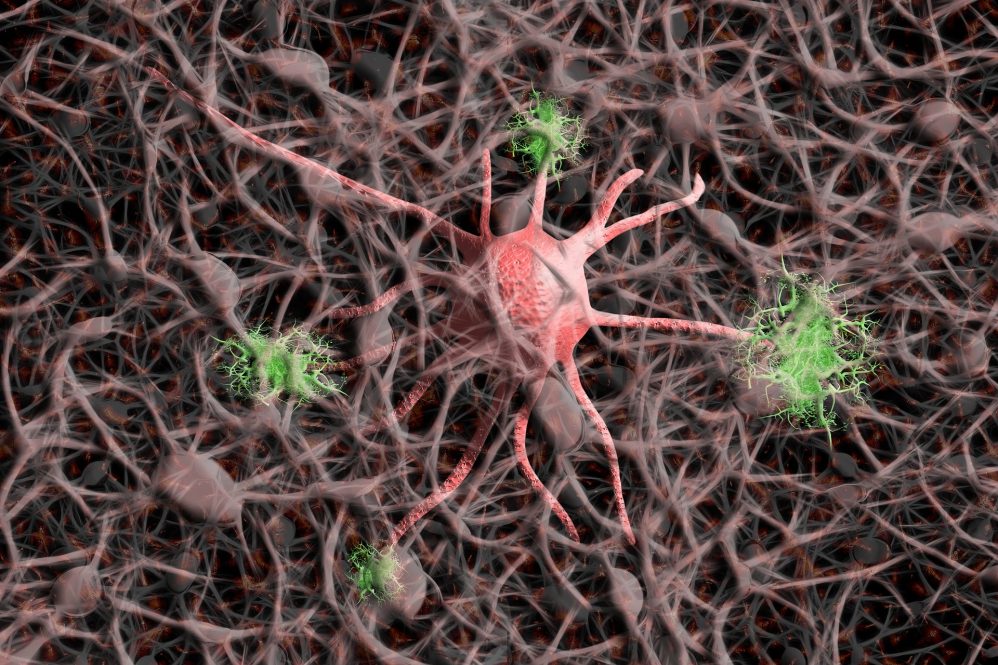
BACE-1 is the primary culprit behind the production of beta-amyloid peptides. These peptides form plaques and are thought to cause the onset and progression of Alzheimer’s Disease. The obvious solution would seem to be inhibiting BACE-1 to prevent these plaques from forming. However, the story is much more complicated.
All clinical trials of BACE-1 inhibitors so far have failed. They found patients taking the inhibitors were experiencing worse cognitive functioning. This is because BACE-1 plays an important role in proper synaptic function.
Synapses are small gaps mediating communication between two neurons in the brain. Our brains work by transmitting signals between neurons across these synapses. Each neuron can have thousands of synapses to support the rapid and constant work of the brain. Synaptic functioning supports everything from sensory detection, muscle movement, and memory.
When a neuron needs to send a message across the synapse, a synaptic vesicle filled with a molecule known as glutamate attaches to the presynaptic membrane. From there, it crosses the synapse and docks on a receptor on the other side. This sets off a chemical reaction that supports long-term potentiation (LTP). LTP is the process through which we form memories, a process that is fundamentally disrupted in patients with Alzheimer’s disease.
BACE-1 plays a role in synaptic vesicle docking so when it is inhibited, less glutamate reaches the receptors and LTP is reduced.
Yan’s team deleted the gene that produced BACE in mouse models and found they had significantly reduced plaque buildup, but also reduced synaptic functioning.
“That data is telling us we do need BACE for normal synaptic functioning,” Yan says. “If we delete BACE, synaptic functioning is reduced.”
The team also tested two commercially available BACE-1 inhibitors from pharmaceutical companies AstraZeneca and Merck. Both drugs had negative impacts on synaptic function.
Das, in the Yan lab, discovered that combining BACE-1 inhibitors with a compound known as mGluR1 positive allosteric modulators (PAMs) can override this effect.
The PAMs bind to another synaptic receptor that sets off the same chemical chain that results in LTP. This approach effectively reduces plaque buildup without sacrificing synaptic functioning.
UConn has patented the novel combination of BACE-1 inhibitors and PAMs as a viable Alzheimer’s Disease treatment through UConn’s Technology and Commercialization Services.
“A combination approach will likely be the most effective for Alzheimer’s treatment,” Yan says.
The researchers will continue to investigate the potential of using PAMs in Alzheimer’s disease treatment. Next, they hope to use Alzheimer’s disease animal models as opposed to the knockout mouse models they used for this study.
UConn Technology Commercialization Services is actively looking for a partner/licensee in the industry to help to move this novel technology out of the lab and into the clinic. To learn more about this technology, contact techcomm@uconn.edu.
Yan holds a Ph.D. in biochemistry from the University of Kentucky and a discoverer of BACE1. His research focuses on understanding Alzheimer’s disease pathogenesis and identifying treatments by investigating the formation of extracellular amyloid-β plaques, mechanism of dystrophic neurite formation in the brain, and exploring reversing neuronal loss.