ImStem Biotechnology, a biopharmaceutical company in UConn’s Technology Incubation Program (TIP), has dosed its first multiple sclerosis (MS) patient with its experimental stem cell drug candidate.
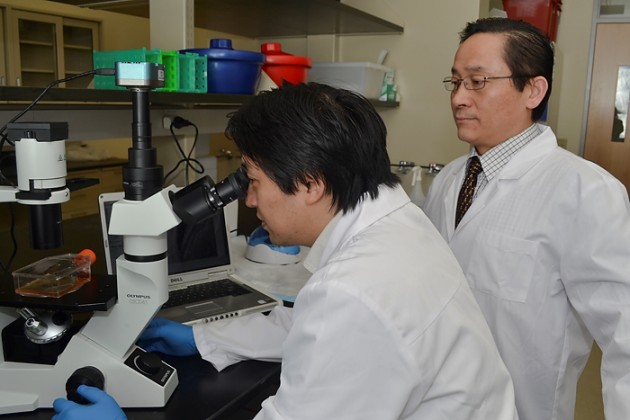
ImStem Biotechnology co-founders Dr. Xiaofang Wang, chief technology officer, and Dr. Ren-He Xu, former director of the UConn Stem Cell Institute developed a drug candidate, IMS001. IMS001 is a human embryonic stem cell-derived mesenchymal stem cell (hES-MSC) therapy.
“We look forward to building a company whose foundation lies in our science based upon years of pioneering research,” said Dr. Xiaofang Wang, Chief Technology Officer of ImStem Biotechnology, and an inventor of the proprietary T-MSC technology.
Mesenchymal stem cells can differentiate into multiple kinds of somatic cells. hEs-MSCs have become an increasingly popular topic for experimental drug treatment research. Because they are derived from human embryonic stem cells, they reduce some of the risks associated with using other animal stem cells, such as transmitting diseases from the cells to the patient or inciting an adverse immune response. Other approaches, such as using bone marrow cells, have limited proliferation and differentiation capacities.
Nearly 1 million people over the age of 18 in the U.S. have been diagnosed with MS. With MS, the immune system attacks the protective layer around nerve fibers known as the myelin, causing inflammation and disrupting communication between the central nervous system and the rest of the body. MS causes physical, mental, and sometimes psychiatric problems. The underlying cause of the disease is still unknown.
IMS001 is delivered to patients intravenously. This drug has the potential to stabilize the blood-brain barrier, based on work by Dr. Joel Pachter at UConn Health. This barrier plays an important role in filtering substances carried by capillaries to the brain to protect the brain. The breakdown of the blood-brain barrier is a hallmark of MS. Repairing this critical mechanism could reduce MS relapse and the progression of disability caused by MS.
The dosing of the first MS patient at the Shepherd Center in Atlanta, Georgia represents the start of ImStem Biotechnology’s ambitious effort to develop an effective treatment for those living with MS.
ImStem Biotechnology’s founders believe this is the first mesenchymal stem cell-based cell therapy accepted by the FDA for a Phase 1 clinical trial.
ImStem Biotechnology plans to enroll a total of 30 patients in this trial. The trials will also test the efficacy of increasing the number of cells dosed per patient.
ImStem Biotechnology plans to continue enrolling patients to test the efficacy of a single dose in MS patients with relapsing-remitting, secondary, or primary progressive MS who have experienced treatment failure with prior disease modifying treatments.
While this clinical trial is focusing on patients with MS, IMS001 could also help treat other neurological, autoimmune, degenerative, and rare orphan diseases with high unmet medical needs.