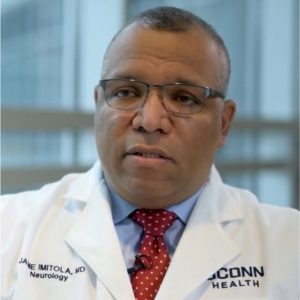
Since we see a lot the patients who are more disenfranchised, with lack of access, and with more co-morbidities, our patients are very sick, as a result of both the biology of the virus and also the inequities of health care. — Dr. Jaime Imitola
Even while hammering home the message of vigilance to protect against the spread of COVID-19, medical experts like Dr. Jaime Imitola acknowledge the growing presence of “COVID fatigue.”
That, he says, has many of us letting our guard down, likely one of several factors contributing to this winter’s spike in COVID-19 infections. Even with the downward trend in the number of infections in recent days and the increase in vaccinations, COVID-19 remains dangerous for many patients, including the chronic immunosuppressed and those with cancer, and the post-acute complications of COVID-19 can cause disability in patients with poor access to health care.
“One collective question for physicians and scientists around the world is how to prepare our population to the constant threat of the infection for the coming years,” Imitola, the director of UConn Health’s Division of Multiple Sclerosis and Translational Neuroimmunology, says. “And we, as the state’s flagship public health institution, have a responsibility to be leaders in the community when it comes to not only treating our patients, but teaching them how to avoid exposure.”
That includes continuing the push for vaccination and boosters and raising awareness of novel alternative pre-exposure prevention options such as Evusheld, a combination of monoclonal antibodies the FDA allowed emergency use of in December.
“In addition to having these tremendous mortalities, what COVID has done in the last two years is unveil this huge gap between all populations, and now we are discovering thousands of COVID survivors with significant neurological, pulmonary and cardiovascular morbidity that will cause added mortality,” Imitola says. “Since we see a lot the patients who are more disenfranchised, with lack of access, and with more co-morbidities, our patients are very sick, as a result of both the biology of the virus and also the inequities of health care.”
Around this time a year ago, Imitola says his MS Center had one patient who was infected with COVID-19 while on immunosuppressive medications for MS. He says a year later there were almost 20.
Of great concern is the notion of complacency, which is not hard to come by with the well-documented success of vaccines and boosters and the perception that the omicron strain largely causes only mild illness. Plus with December’s holiday gatherings, after nearly two years, people may have been more likely to relax their precautions. All those factors combined, while they may not always pose a substantial threat to young, healthy, fully vaccinated people — still can be devastating for someone on MS medications or with cancer.
“Patients with a compromised immune system cannot mount a humoral response, so they don’t have a rapid response to the virus,” Imitola says. “Therefore the virus is going to have more time to replicate and yield more damage and injury, and more activation of the immune system’s other cells that are injurious to the body.”
Endemic infections remain a threat and are still deadly. One of the less anticipated sufferings from COVID-19 is the long-term consequences that can be equally devastating for people. — Dr. Jaime Imitola
He likens the immune response — the humoral response along with the T-cell response — to an army and navy working together to attack the invading virus.
“Now in patients who are immunocompromised, they may have the army only, but they don’t have the navy so complete, and that’s why they’re at risk for getting sicker,” Imitola says. “If you put on top of that — things like diabetes, hypertension, old age, asthma — then what the coronavirus does is, it’s like an accelerant to a fire, it becomes bigger and faster, and that’s when people get really, really sick almost immediately. And if you’re a minority, you live in close quarters, and you have these comorbidities, you’re going to be at an even higher risk, and on top of that, if you’re in an immunocompromised state, you’re very, very fragile and very, very at risk of getting a virus that may not kill everybody, but in your case, it will kill you.”
“As a leading medical school and hospital, we need to remain engaged with our communities, especially the poor and disenfranchised, to provide education about risk-mitigation strategies.”
Crucial to that is dispelling misinformation that can encourage complacency from the belief that as COVID-19 becomes endemic, or constantly present, it’s less problematic.
“This doesn’t mean that the infection is over,” Imitola says. “Endemic infections remain a threat and are still deadly. One of the less anticipated sufferings from COVID-19 is the long-term consequences that can be equally devastating for people. Those challenges are why UConn Health offers care and research from the Long-COVID Recovery Center, led by Dr. Ameer Rasheed.”
So the advice is to be resilient against the temptation of complacency and to maintain the precautions, as draining and frustrating as they may be. For the immunocompromised, that means more of the same — keep up with the recommendations for vaccination and boosters, avoid gatherings, and wear masks. And, for their protection, the rest of us still might consider continuing to take those steps too.



