Women over the age of 45 or who have had children may undoubtedly know that feeling when the urge to “go” and “go now” comes on or the sudden leak that occurs with a sneeze or a jump in an aerobics class. Others may feel something bulging from the vagina when they are straining.
If you’ve experienced this, you may think that it’s just part of aging or being a woman. The good news is, it’s not and the new urogynecology specialist at UConn Health can solve those problems and help your quality of life.
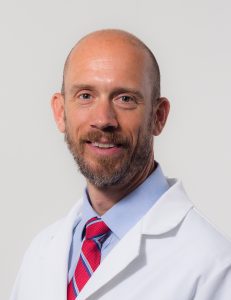
Dr. Jonathan Shepherd, urogynecologist and professor of medicine joined UConn Health’s Women’s Center last summer, specializing in treating women with urinary incontinence, pelvic organ prolapse, and disorders that affect the bladder, reproductive organs, and bowels, which can affect a quarter of women.
“Twenty-five percent of women may have one or more pelvic floor disorders,” says Shepherd. “However, there are treatments so you don’t have to live with them.”
PROLAPSE
Pelvic organ prolapse happens when one or more pelvic organs (the vagina, uterus, bladder, small intestine, and rectum) drop from their normal position. It’s caused by a weak pelvic floor, the collection of muscles, ligaments, and connective tissues that hold these organs in place.
“Prolapse and incontinence affect 1 in 4 women and happens twice as often as breast cancer, but because it has been socially taboo, people tend not to talk about it,” says Shepherd.
Pelvic organ prolapse is caused by anything that puts increased pressure on the abdomen. The most common cause is childbirth, however, obesity, chronic cough, constipation, and genetics are other causes.
Some women have no symptoms at all, but others report a feeling of pressure in the pelvic area, a feeling that something is falling out of the vagina. Others also have urinary leakage or chronic urge to urinate, constipation, or loss of bowel control.
There are non-surgical treatment options for most types of pelvic organ prolapse which include pelvic floor physical therapy and/or the use of a pessary, a vaginal support device.
Pelvic floor physical therapy, which is vastly different than typical physical therapy is also done in the OB/GYN department by a specialized physical therapist, who helps patients learn to contract and relax the pelvic floor muscles relative to other muscles.
The exercises are designed to stretch tight muscles, strengthen weak muscles and boost flexibility.
The pessary is a vaginal support device similar to a vaginal contraceptive diaphragm that expands to lift the bladder and hold it in place. This is a low-risk treatment and the patient does not feel the device.
Surgery may be necessary for some and Shepherd performs minimally invasive surgery either through the vagina or laparoscopically. Depending on the type of prolapse either a patient’s own ligaments or mesh is used to lift and reinforce the tissue. A hysterectomy may also be an option for those who no longer plan to have children and the prolapse is at the top of the vagina.
INCONTINENCE
While incontinence is more common as we age, it is not a normal part of aging. There are many different treatment options available, which can have a positive impact on the quality of your life.
Stress incontinence and urgency incontinence affect many women but tend to be embarrassing and not discussed. These types of incontinence can be caused by pregnancy and childbirth, menopause, pelvic surgery, or weakened muscles around the bladder. Most women experience a combination of both stress incontinence and urgency incontinence.
There are treatment options for both types of incontinence. Although your primary care physician, OB/GYN, or urologist may also treat these problems, a urogynecologist offers additional expertise.
Women no longer need to stop doing the things they love for fear of “the leak.”
Stress Incontinence
Stress Incontinence happens during physical activity, straining, or exertion. Women may experience urine leakage, especially when coughing, laughing, exercising, or sneezing.
Up to 90% of cases of female incontinence are successfully treated, however, there currently is no medication for stress incontinence. Pelvic floor muscle exercises often referred to as Kegels are considered first-line treatments for stress incontinence. A pelvic floor physical therapist can help coach women on how to properly do Kegels to strengthen the pelvic muscles.
Electrical stimulation can also help muscles as well as biofeedback to record the progress of strengthening treatments and exercises.
When other options do not work, sling surgery is the most common surgery doctors use to treat urinary stress incontinence. The surgeon creates a sling out of mesh or human tissue and puts it under the urethra where the urine passes through. The sling acts like a hammock to lift and support the urethra to help prevent leaks.
Urgency Incontinence
Urgency incontinence also called overactive bladder is when there is a need to urinate frequently and leakage may also happen, however when the urge comes on, it’s pretty urgent to find a restroom.
Medications that relax the bladder can help relieve symptoms of overactive bladder and reduce episodes of urge incontinence.
If medications do not work to solve urge incontinence another option is bladder stimulation. A device much like a pacemaker would be used for the heart is implanted under the skin at the buttocks and stimulates the nerves of the bladder. Electrical stimulation sends a mild electric current to nerves in the lower back or the pelvic muscles that are involved in urination.
Botox is another option to treat urge incontinence or overactive bladder in people who have not had success with other treatment options. The Botox is injected into the bladder and helps the muscles relax, which takes away the urgency and allows more time to get to the bathroom. Most people get symptom relief quickly in as short as a few days. The treatment results need to be repeated yearly.
You don’t need to live with these uncomfortable issues. Speak with a urogynecologist at the UConn Health Women’s Center and find out how to improve your quality of life by treating your incontinence or prolapse issues.