A trip to the Emergency Department at UConn John Dempsey Hospital for severe jaundice led to a diagnosis of a bile duct blockage for Jay Buth of Avon. After some further research, a stent was placed in the bile duct and his gall bladder was removed.
When the stent was removed from his bile duct, it collapsed and he ended up back in the Emergency Department where a CT Scan was performed and incidentally found a visible mass on Buth’s pancreas.
Buth followed up with Dr. Murali Dharan, assistant professor of Gastroenterology at UConn Health who ordered a PET scan. The PET scan indicated that the tumor was at a very early stage and was localized to the pancreas providing a good prognosis.
“What I love about UConn Health was that they kept looking and were not satisfied until they found the answer,” says Buth.
During digestion, your pancreas makes pancreatic juices called enzymes. These enzymes break down sugars, fats, and starches. Your pancreas also helps your digestive system by making hormones. Pancreatic cancer is a type of cancer that starts in the pancreas and pancreatic adenocarcinoma is the most common type of pancreatic cancer.
Risk factors for pancreatic cancer include:
- Tobacco use
- Being overweight
- Diabetes
- Chronic pancreatitis
- Workplace exposure to certain chemicals
- Age – Almost all patients are older than 45. About two-thirds are at least 65 years old. The average age at the time of diagnosis is 70.
- Gender- Men are slightly more likely to develop pancreatic cancer than women.
- Race – African Americans are slightly more likely to develop pancreatic cancer than whites.
- Family history
- Inherited genetic syndromes
Symptoms:
- Abdominal pain that radiates to your back.
- Loss of appetite or unintended weight loss.
- Yellowing of your skin and the whites of your eyes (jaundice)
- Light-colored stools.
- Dark-colored urine.
- Itchy skin.
- New diagnosis of diabetes or existing diabetes that’s becoming more difficult to control.
- Blood clots.
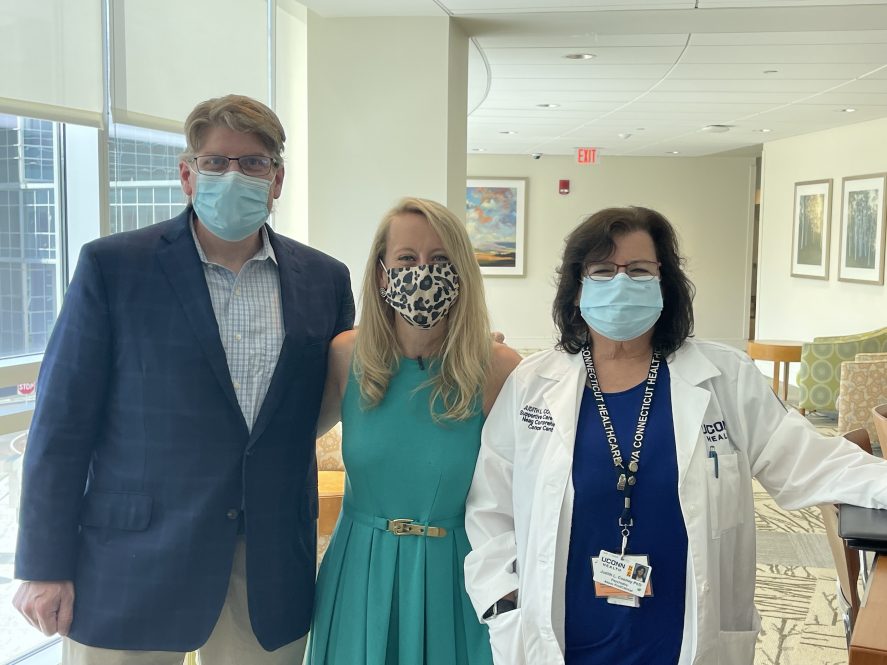
Buth met with Dr. Pragna Kapadia, assistant professor of the Department of Medicine Hematology and Medical Oncology Division at the Carole and Ray Neag Comprehensive Cancer Center at UConn Health and Dr. David McFadden, professor and chair of the Department of Surgery at UConn Health to determine his treatment plan.

Buth started what would be eight rounds of chemotherapy which will be followed by a chemo-radiation combination. He was fortunate that he didn’t have major side effects from the chemotherapy which included five hours at the infusion center and another 48 hours at home.
“Besides cancer, I was in the best shape of my life,” says Buth.
From there, Buth will have a Whipple procedure (pancreaticoduodenectomy) this summer. This is the most common operation to remove cancer in the head of the pancreas. During this operation, the surgeon removes the head of the pancreas and sometimes the body of the pancreas as well. Nearby structures such as part of the small intestine, part of the bile duct, the gallbladder, lymph nodes near the pancreas, and sometimes part of the stomach are also removed. The remaining bile duct and pancreas are then attached to the small intestine so that bile and digestive enzymes can still go into the small intestine. The end pieces of the small intestine (or the stomach and small intestine) are then reattached so that food can pass through the digestive tract (gut).
Judith Cooney PhD, health psychologist and associate professor of Psychiatry at the Cancer Center at UConn Health practices health psychology, a specialty area that applies psychological principles and evidence-based treatments to help manage the psychosocial impact of medical and health problems and to change health behaviors.
In health psychology, Cooney works with cancer patients at all phases of treatment to help cope with cancer, evaluation and diagnosis, treatment, and post-acute treatment during survivorship to return to life and thrive following cancer.
“Often survivorship is the chapter in the cancer journey that gets the least support,” says Dr. Cooney. “It’s a transformative and frightening time after cancer changed their life.”
Cooney has been working with Buth to help him cope with the distress of his challenging cancer diagnosis, and his difficult acute treatment phases and their work will continue to the post-treatment phase.
“Mr. Buth has been amazing in learning ways to manage distress and transform and grow through cancer,” says Cooney. “His story is inspirational.”
Buth who sees Cooney weekly says “She is amazing and has helped me on a host of levels beyond cancer.”
Buth now has a new perspective on life, focusing on the little things, the important people in his life, and finding joy in everything. He credits the tools in the “tool kit” that Cooney provided him with getting through this with a positive outlook.
“Had I not had issues with the gall bladder that tried to kill me, we may not have found this so early, it actually saved me,” says Buth. “We would be having a very different conversation now had it not been found so early.”
“I am over the moon with the care at UConn, it is world-class,” says Buth. “I love the nurses and cannot say enough about how wonderful they are – they do God’s work.”