For years, the left leg of Maureen Previti, 78, of Broad Brook, Conn. kept getting more and more swollen.
As a now proud 4 ft. 10.5 in. woman, who used to stand 5 ft. high, she closely watched her sodium intake, tried diuretic medications, and often elevated her leg non-stop to curb the swelling.

“For two years doctors kept testing my left leg to find out why it was swelling but with no answers,” reports Previti. “My leg kept getting bigger and bigger. I never have had long legs but as a former dancer I always valued my legs.”
She even had to begin buying two different sized shoes, and her leg skin would also get major irritation and indentations. She had been tested multiple times with heart and vein ultrasound without learning any answers.
“I know my body and there just had to be a reason for my leg swelling.”
Her UConn Health dermatologist Dr. Marti Rothe took one look at Previti’s leg and referred her to ‘a great UConn Health heart doctor!’
Turns out with that simple referral Previti’s mysterious leg swelling was soon about to be finally solved.
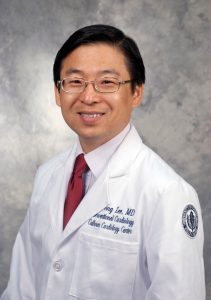
“There is a special detective at UConn Health named Dr. JuYong Lee!’ exclaims Previti. “He thinks out of the box. UConn is a teaching hospital. I knew they would be able to think out of the box to find a solution for me.”
Within days of meeting Lee at the Calhoun Cardiology Center the interventional heart doctor fixed her leg on December 24, 2022 by inserting one iliac vein stent to open up her compressed vein to restore proper blood flow and drainage capability in her left leg.
“Believe it or not – my leg was perfect in two days,” says Previti. “Prior to my vein stent procedure I hadn’t seen my ankle in two years!”
“I am so happy Maureen was able to undergo a successful evaluation and treatment with left iliac vein stenting,” says Lee, director of Vascular Medicine/Endovascular Medicine and the director of Structural Heart Program at UConn Health. “She has a dramatic improvement of her leg swelling that she suffered many years. Intravascular ultrasound tests confirmed significant partial blockage of her iliac vein and required stenting which led to significant improvement of her left leg painful edema.”
Previti is thrilled to have her mobility and quality of life finally restored as she is set to turn 79 this August 9, and perhaps she will even soon get back to her love of dancing every Friday and Saturday night.

“The procedure worked so well and it even made me happier. Dr. Lee has turned back time for me and my leg, and has put a true happy smile on my face,” says Previti happily.
“When it comes to my health care for something important, I head to UConn Health. I know they are always going to innovatively care for me,” she says. “Plus, UConn’s doctors like Dr. Lee are not only good, but so kind too!”
According to Lee, patients like Previti experiencing major swelling of their lower extremities can often suffer from skin conditions such as dermatitis or cellulitis. Often, as a result they experience skin infections, fail to respond to diuretic drug regimens, require recurrent emergency room visits and undergo repeated venous duplex ultrasound studies, without identification of the underlying causes of their chronic edema.
That’s why Lee started a Chronic Leg Edema Program at UConn Health to help these patients.
“Our new strategy for severe leg edema is to use systemic diagnostic and therapeutic approaches for each patient to delineate the possible causes for each particular patient’s leg swelling, as leg edema is not caused simply by one disease condition, but multiple diseases can be causing it,” says Lee. “As a cardiologist and also a vascular medicine physician, I have the ability to leverage multiple minimally invasive tests such as right heart catheterization to rule out undiagnosed diseases such as heart failure or pulmonary hypertension and use peripheral vein intravascular ultrasound with venography. I can rule out or rule in all the various causes of a patient’s leg edema in just one elective outpatient diagnostic procedure visit and to identify any present vein compression or insufficiency culprits to intervene.”
While most vascular programs are focused on diseases of the peripheral arteries, Lee’s program is filling an important clinical need.
“I noticed that peripheral venous issues of patients were not being well addressed in clinical practice. This realization led me to develop a comprehensive peripheral venous therapy program here at UConn Health,” says Lee. “As a result, an increasing number of patients with refractory chronic leg edema and stasis dermatitis have been referred to me from different specialties for assessment.”
Venous blockages or compressed and/or impaired veins can cause drainage and improper blood flow issues going from the leg and back to the heart. It also can cause not only severe swelling and skin changes, but places a patient at increased risk of potentially life-threatening complications such as deep vein thrombosis (DVT) and pulmonary embolism.
In fact, in February 2022 Lee presented his clinical 2018-2020 patient data study findings about 38 refractory leg edema patients he evaluated and treated during the Annual Meeting of the American Venous Forum, a non-profit academic society dedicated to improving the care of patients with venous and lymphatic disease. Interestingly, 34.2 percent of these patients were revealed to have a iliac vein lesion such as a vein partial compression blockage which is a much higher incidence in this particular patient group of chronic refractory leg swelling compared to the general population. Also, more interestingly, the etiology was found to be frequently multifactorial. Venous insufficiency with previously undiagnosed diastolic congestive heart failure was the most common in 26% of patients and venous insufficiency with partial iliac vein compression blockages in 18.4%. This data showed that the refractory leg edema patient needs to be cared for with a systemic approach as the causes of the condition is often not one but multiple conditions.
Lee has even developed a new clinical Leg Edema Diagnostic/Therapeutic Algorithm to help increase the chances of making an accurate diagnosis for patients with chronic edema so they can be treated with an effective and targeted therapeutic plan. Lee is training his clinical fellows to apply the Algorithm in their future practice and also educating referring physicians, so their patients don’t suffer for years with unknown leg swelling.
“Chronic venous hypertension and painful leg edema is a challenging diagnosis to make. But once we identify the causes through this algorithm, it is mostly treatable with using combined targeted therapy depending on the causes such as management of newly diagnosed heart failure or pulmonary hypertension through right heart catheterization, or even curable with iliac vein stenting if the main cause is the vein’s partial blockage.”
Lee stresses: “Our patients at UConn Health are experiencing significant clinical symptoms improvement for lifelong refractory leg edema with combined therapeutic approaches with vein stenting, venous ablation and appropriate medical therapy depending on the causes found from this systemic collective diagnostic approach effectively, or even miraculously as some patients report” he says.